Deep Neck Space Infection Mini LCTR
Diunggah oleh
medinoJudul Asli
Hak Cipta
Format Tersedia
Bagikan dokumen Ini
Apakah menurut Anda dokumen ini bermanfaat?
Apakah konten ini tidak pantas?
Laporkan Dokumen IniHak Cipta:
Format Tersedia
Deep Neck Space Infection Mini LCTR
Diunggah oleh
medinoHak Cipta:
Format Tersedia
Agung D. Permana,dr.,M.Kes.
,SpTHT-KL
Deep Neck Space Infection
Introduction
DEEP NECK SPACE INFECTIONS
Life threatening
delay in diagnosis/inadequate/inappropriate treatment
complications mortality rates : 40%
head and neck surgeon :
cervical fascias & potential spaces understand the
treatment & potential complications
antibiotics decreased the incidence and mortality
Anatomy Of The Cervical Fascia
Superficial cervical fascia
Deep cervical fascia
1. Superficial layer
2. Middle layer
- Muscular division
- Visceral division
3. Deep layer
- Prevertebral division
- Alar division
Sternocleidomastoid
Trapezius
Deep Cervical Fascia
Investing layer of deep cervical fascia
Prevertebral fascia
Pretracheal fascia
(visceral part)
Carotid sheath
Buccopharyngeal fascia
Alar fascia
Pretracheal fascia
(muscular part)
T
E
Cervical Fascia
Pathophysiology
Deep neck space infections can arise from a multitude of causes.
Whatever the initiating event, development of a deep neck space
infection proceeds by one of several paths, as follows:
Spread of infection can be from the oral cavity, face, or superficial
neck to the deep neck space via the lymphatic system.
Lymphadenopathy may lead to suppuration and finally focal
abscess formation.
Infection can spread among the deep neck spaces by the paths of
communication between spaces.
Direct infection may occur by penetrating trauma.
Sign And Symptoms
Mass effect of inflamed tissue or abscess cavity
on surrounding structures
Direct involvement of surrounding structures
with the infectious process
Presentation
Obtain a detailed history from patients in whom deep neck space
infection is suspected. Eliciting a history of the following is
important:
Pain
Recent dental procedures
Upper respiratory tract infections (URTIs)
Neck or oral cavity trauma
Respiratory difficulties
Dysphagia
Immunosuppression or immunocompromised status
Rate of onset
Duration of symptoms
Retropharyngeal Space Infection
Source
Nose
Sinuses
Adenoids
Nasopharynx
Manifestations
Acute URTI in infants & children
Dysphagia & odynophagia
Drooling & difficult to expell excretions
Cervical rigidity
Muffled voice
Dyspnea
Unilateral bulging of posterior pharyngeal wall
Sepsis
Retropharyngeal Space Infection
Pediatrics
"Cause > suppurative process in lymph nodes
#Nose, adenoids, nasopharynx, sinuses!
Adults
Cause > trauma, instrumentation, extension
adjoining deep neck space
Danger Space Infection
Source
Retropharyngeal space
Prevetebral space
Parapharyngeal space
Manifestations
Same as primary space infection
Severe sepsis
Treatment
Same as for primary space infection
Complications
Potential for rapid spread through the loose areolar tissue
Inferior spread to the posterior mediastinum to the level of diafragma
Prevertebral Space Infection
Manifestations
Midline abcess
Cold abcess posterior pharynx
Slow spread of suppuration of this area
Treatment
Needle aspiration w/ subsequent antituberculosis th/
Stabilization of spine
Source
Vertebral bodies
Penetrating injuries
Tuberculosis of the spine
Complications
Spine instability progression of vetebral process
Visceral Vascular Space Infection
potential space within the carotid sheath
infections remain relatively localized
compact space contains little areolar
connective tissue
lymphatics contained within this space receive
secondary drainage from most of the
lymphatics of the head and neck
Lincoln Highway of The Neck (Mosher) all
three layers of the DCF contribute to the
carotid sheath
Visceral Vascular Space Infection
Source
Parapharyngeal space
Submandibular space
Visceral space
Manifestations
Pitting edema over SCM
Torticollis
Treatment
External drainage
I.V. antibiotics
Possible ligation of IJV
Complications
Septic shock
Carotid artery erotions
Endocarditis
Cavernous sinus
thrombosis
Pharingomaxillary Space Infection
Prestyloid Compartement [anterior-muscular]
Fat
Lymph nodes
Internal maxilarry artery
Inferior alveolar, lingual,auriculotemporal nerves
Poststyloid Compartement [posterior-neurovascular]
Carotid artery
Internal jugular vein
Symphatetic chain
IX, X, XI, XII nerves
Pharingomaxillary Space Infection
Source
Tonsil
Pharynx
Teeth
Temporal bone (petrous)
Parotis gland
Lymph nodes of nose &
nasopharynx
Manifestations
Medial displacement of lateral
pharyngeal wall and tonsils
Trismus
Parotid edema
Retromandibular neck fullness
Dysphagia
Peritonsillar Space Infection
Source
Tonsils & pharynx
Manifestations
Dysphagia/odynophagia
Drooling and hot potato voice
Muffleed voice
Reffered otalgia
Trismus
Displaced tonsil toward midline
Deviated uvula
Submandibular Space Infection
Sublingual space
Sublingual gland
Hypoglossal nerve
Whartons ducts
Submaxillary space
Central compartement
Submental compartement
Submaxillary compartement
subdivided by anterior bellies of
digastric m.
Contents
Submandibular gland
Lymph nodes
Submandibular Space Infection
Source
Teeth
Salivary glands
Pharynx & tonsils
Sinuses
Manifestations
Dysphagia
Odynophagia
Treatment
Underlying pathology
External drainage if it progress
- sublingual
- submandibula
Complications
Ludwigs Angina
Ludwigs Angina
Ludwigs angina
Masticator Space Infection
Source
Molar teeth
Manifestations
1. Extreme trismus
2. Edema & tenderness over
the posterior ramus of
mandible
Treatment
External drainage
Temporal Space Infection
Temporalis m. :
- superficial compartments
- deep compartments
Manifestation
Pain in this area Trismus
Treatment
External drainage
Anterior Visceral Space
Contents
Pharynx
Esophagus
Larynx
Trachea
Thyroid gland
Source
Tonsils
Esophageal injury
Blunt trauma w/ mucosal tear
Acute thyroiditis
Chest infection
Anterior Visceral Space
Microbiology
Preantibiotic eraS.aureus
Currentlyaerobic Strep species and non-strep
anaerobes
Gram-negatives uncommon
Almost always polymicrobial
Remember resistance !!!
Imaging
Lateral neck plain film
"Screening exammainly for retropharyngeal and
pretracheal spaces
"Normal: 7mm at C-2, 14mm at C-6 for kids,
22mm at C-6 for adults
Imaging
Imaging
High-resolution Ultrasound
"Advantages
Avoids radiation
Portable
"Disadvantages
Not widely accepted
Operator dependent
Inferior anatomic detail
"Uses
Following infection during therapy
Image guided aspiration
Imaging
Contrast enhanced CT
"Advantages
Quick, easy
Widely available
Familiarity
Superior anatomic detail
Differentiate abscess and cellulitis
"Disadvantages
Ionizing radiation
Allergenic contrast agent
Soft tissue detail
Artifact
Imaging
MRI
"Advantages
No radiation
Safer contrast agent
Better soft tissue detail
Imaging in multiple planes
No artifact by dental fillings
"Disadvantages
Increased cost
Increased exam time
Dependent on patient cooperation
Availability
Treatment
Airway protection
Antibiotic therapy
Surgical drainage
Airway protection
"Observation
"Intubation
Direct laryngoscopy: possible risk of rupture and
aspiration
Flexible fiberoptic
"Tracheostomy
Ideally = planned, awake, local anesthesia
Abscess may overlie trachea
Distorted anatomy and tissue planes
Treatment
Antibiotic Therapy
"Polymicrobial infections
Aerobic Strep, anaerobes
Ampicillin/sulbactam with metronidazole
"Beta-Lactam resistance in 17-47% of isolates
"Alternatives
Third generation cephalosporins
clindamycin
"Culture and sensitivity
Treatment
Surgical Drainage
Transoral
Preoperative CT where are the great vessels? CT
Cruciate mucosal incision, blunt spreading through superior
pharyngeal constrictor
External drainage
Surgical Drainage
"External
EXPOSURE, EXPOSURE!!!
approach
Submandibular incision
Submental incision
T-incision
Complication
Airway obstruction
Ruptured abscess
Internal Jugular Vein Thrombosis
Carotid artery Rupture
Mediastinitis
history
Physical examination
Secure airway
Culture, IV antibiotic
CT scan
Small abcess
Needle aspiration
for culture and drainage
Impending complication ?
No abcess Large abcess
Watch and wait
24-48 hours
Clinical improvement ?
Continue antibiotic,
Needle aspirations
Surgical incision
And drainage
No
Yes
Yes
No
Pharingomaxillary Space Infection
Treatment
External drainage
Tracheotomy
Complications
Septic thrombosis of IJV
Carotid artery erosions
Cranial nerve involvement
Mediastinitis
Peritonsillar Space Infection
Treatment
Peroral drainage
tonsilectomy
Complications
Spread into pharyngomaxilary
space through posterior
pharyngeal wall
Retropharyngeal Space Infection
Treatment
1. Fasting
2. I.V. antibiotics
3. Tracheotomy
4. Emergent surgical drainage
- intraoral drainage
- external drainage
Complications
1. Rupture of abcess w/
aspiration & pneumonia
2. Mediastinitis
3. Airway obstruction
PMS
Masticator
Submandibular
Peritonsillar
VVS
Danger
Mediastinum Anterior Visceral
Temporal
Parotid
Prevertebral
Retropharingeal
Pharingomaxillary Space Infection
Anda mungkin juga menyukai
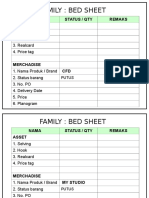
- Family: Bed Sheet: Nama Status / Qty Remaks AssetDokumen19 halamanFamily: Bed Sheet: Nama Status / Qty Remaks AssetmedinoBelum ada peringkat
- AlfiDokumen1 halamanAlfimedinoBelum ada peringkat
- Lecture1 - General ParasitologyDokumen40 halamanLecture1 - General ParasitologymedinoBelum ada peringkat
- Basic Examination of BloodDokumen48 halamanBasic Examination of BloodmedinoBelum ada peringkat
- CH 3 StoichiometryDokumen30 halamanCH 3 StoichiometrymedinoBelum ada peringkat
- Introduction To HemostasisDokumen45 halamanIntroduction To Hemostasismedino100% (3)
- Health Care Waste Hospital Waste: Public Health Department Faculty of MedicineDokumen34 halamanHealth Care Waste Hospital Waste: Public Health Department Faculty of MedicinemedinoBelum ada peringkat
- Shoe Dog: A Memoir by the Creator of NikeDari EverandShoe Dog: A Memoir by the Creator of NikePenilaian: 4.5 dari 5 bintang4.5/5 (537)
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeDari EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifePenilaian: 4 dari 5 bintang4/5 (5794)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceDari EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RacePenilaian: 4 dari 5 bintang4/5 (895)
- The Yellow House: A Memoir (2019 National Book Award Winner)Dari EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Penilaian: 4 dari 5 bintang4/5 (98)
- Grit: The Power of Passion and PerseveranceDari EverandGrit: The Power of Passion and PerseverancePenilaian: 4 dari 5 bintang4/5 (588)
- The Little Book of Hygge: Danish Secrets to Happy LivingDari EverandThe Little Book of Hygge: Danish Secrets to Happy LivingPenilaian: 3.5 dari 5 bintang3.5/5 (400)
- The Emperor of All Maladies: A Biography of CancerDari EverandThe Emperor of All Maladies: A Biography of CancerPenilaian: 4.5 dari 5 bintang4.5/5 (271)
- Never Split the Difference: Negotiating As If Your Life Depended On ItDari EverandNever Split the Difference: Negotiating As If Your Life Depended On ItPenilaian: 4.5 dari 5 bintang4.5/5 (838)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyDari EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyPenilaian: 3.5 dari 5 bintang3.5/5 (2259)
- On Fire: The (Burning) Case for a Green New DealDari EverandOn Fire: The (Burning) Case for a Green New DealPenilaian: 4 dari 5 bintang4/5 (74)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureDari EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FuturePenilaian: 4.5 dari 5 bintang4.5/5 (474)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryDari EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryPenilaian: 3.5 dari 5 bintang3.5/5 (231)
- Team of Rivals: The Political Genius of Abraham LincolnDari EverandTeam of Rivals: The Political Genius of Abraham LincolnPenilaian: 4.5 dari 5 bintang4.5/5 (234)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaDari EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaPenilaian: 4.5 dari 5 bintang4.5/5 (266)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersDari EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersPenilaian: 4.5 dari 5 bintang4.5/5 (345)
- The Unwinding: An Inner History of the New AmericaDari EverandThe Unwinding: An Inner History of the New AmericaPenilaian: 4 dari 5 bintang4/5 (45)
- Rise of ISIS: A Threat We Can't IgnoreDari EverandRise of ISIS: A Threat We Can't IgnorePenilaian: 3.5 dari 5 bintang3.5/5 (137)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreDari EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You ArePenilaian: 4 dari 5 bintang4/5 (1090)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)Dari EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Penilaian: 4.5 dari 5 bintang4.5/5 (121)
- Her Body and Other Parties: StoriesDari EverandHer Body and Other Parties: StoriesPenilaian: 4 dari 5 bintang4/5 (821)
- MFA EXIT EXAM QUESTIONS AND ANSWERS 1.0 Part ADokumen5 halamanMFA EXIT EXAM QUESTIONS AND ANSWERS 1.0 Part ADiptendu ParamanickBelum ada peringkat
- RH Incompatibil TY: What Is RH Incompatibility?Dokumen15 halamanRH Incompatibil TY: What Is RH Incompatibility?Jannah Marie A. DimaporoBelum ada peringkat
- Usher Syndrome Awareness DayDokumen10 halamanUsher Syndrome Awareness DayakankshaBelum ada peringkat
- Hyperbilirubinemia ManagementDokumen37 halamanHyperbilirubinemia ManagementkaerickaericBelum ada peringkat
- Addison's Syndrome DiseaseDokumen2 halamanAddison's Syndrome DiseaseNP YarebBelum ada peringkat
- Jaundice NeonatalDokumen26 halamanJaundice Neonatalhunk2662Belum ada peringkat
- MastitisDokumen12 halamanMastitismanal at100% (1)
- Lapkas Marasmus JadiDokumen48 halamanLapkas Marasmus JadiRivhan FauzanBelum ada peringkat
- Pamphlet InsideDokumen1 halamanPamphlet Insideapi-2408549370% (1)
- HIVAIDS Kaposi Sarcoma A Practical ApproachDokumen55 halamanHIVAIDS Kaposi Sarcoma A Practical ApproachAndrei CluBelum ada peringkat
- Cleocin - Side Effects, Uses & DosageDokumen4 halamanCleocin - Side Effects, Uses & Dosagetarun yadavBelum ada peringkat
- Vats Yustinus Rurie WirawanDokumen6 halamanVats Yustinus Rurie Wirawanrurie wirawanBelum ada peringkat
- Anatomy Liver FlukeDokumen3 halamanAnatomy Liver Flukeapi-295865391Belum ada peringkat
- Diagnostic & Treatment Breast Carcinoma: Dr. Dr. Effif Syofra Tripriadi, Sp. B (K) OnkDokumen64 halamanDiagnostic & Treatment Breast Carcinoma: Dr. Dr. Effif Syofra Tripriadi, Sp. B (K) OnkfebriantaraBelum ada peringkat
- Edited Insecticidal Efficacy and Repellency of OreganoDokumen9 halamanEdited Insecticidal Efficacy and Repellency of OreganoChu Gabriel100% (1)
- Endometriosis: by Jane LyttletonDokumen8 halamanEndometriosis: by Jane Lyttletonitsik12886Belum ada peringkat
- Republic of The Philippines DOH Regional Office XIII Butuan City Midwife Ii Narrative ReportDokumen1 halamanRepublic of The Philippines DOH Regional Office XIII Butuan City Midwife Ii Narrative ReportLAURENCE ALBIOSBelum ada peringkat
- 2020.02.11 New Hospital Order Format Feb 14-23Dokumen4 halaman2020.02.11 New Hospital Order Format Feb 14-23Stib BrionesBelum ada peringkat
- Prescribing Information: (Methoxsalen, USP)Dokumen9 halamanPrescribing Information: (Methoxsalen, USP)Jeliny Bintan MaisuriBelum ada peringkat
- IntussusceptionDokumen2 halamanIntussusceptionAireen Mae P. NapigkitBelum ada peringkat
- LV Systolic FunctionDokumen36 halamanLV Systolic Functionsruthimeena6891Belum ada peringkat
- NCP Decrease Cardiac OutputDokumen2 halamanNCP Decrease Cardiac OutputAnonymous 2hJKVrBelum ada peringkat
- AldosteronismDokumen48 halamanAldosteronismMiguel Cuevas DolotBelum ada peringkat
- Bacterial Causes of URIDokumen28 halamanBacterial Causes of URIOmar MohammedBelum ada peringkat
- Formula For Calculating The IV Flow RateDokumen16 halamanFormula For Calculating The IV Flow Rateblythe RiveroBelum ada peringkat
- Medical Problems and Injuries British English TeacherDokumen5 halamanMedical Problems and Injuries British English TeacherTanitaBelum ada peringkat
- Related Teenshealth Links: Health Problems SeriesDokumen13 halamanRelated Teenshealth Links: Health Problems SeriesMario BadayosBelum ada peringkat
- Tachdjian's Pediatric Orthopaedics v.4Dokumen660 halamanTachdjian's Pediatric Orthopaedics v.4Leonardo Garay QuinteroBelum ada peringkat
- Medsurg 3 Exam 1Dokumen55 halamanMedsurg 3 Exam 1Melissa Blanco100% (1)
- Agent JohnsonDokumen1 halamanAgent JohnsonJulio Cesar PerezBelum ada peringkat