Membantu Pasien Dengan Gejala Dan Membawaa Produk Obat
Diunggah oleh
Misgi Candra Dasa0 penilaian0% menganggap dokumen ini bermanfaat (0 suara)
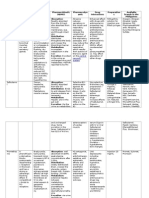
9 tayangan13 halaman1. The document discusses various frameworks for structuring patient consultations, including mnemonics to guide questioning (WHAM, ASMETHOD) and categories for documenting outcomes of treatment (resolved, stable, improved, etc.).
2. It provides examples of using each outcome category in clinical cases, such as describing a pneumonia being resolved after antibiotic treatment or hypertension stabilized with medication.
3. The final outcomes discussed are worsened, failure, and expired, with examples of when a change in treatment is needed or a patient passes away during therapy.
Deskripsi Asli:
asfasafa
Hak Cipta
© © All Rights Reserved
Format Tersedia
PPTX, PDF, TXT atau baca online dari Scribd
Bagikan dokumen Ini
Apakah menurut Anda dokumen ini bermanfaat?
Apakah konten ini tidak pantas?
Laporkan Dokumen Ini1. The document discusses various frameworks for structuring patient consultations, including mnemonics to guide questioning (WHAM, ASMETHOD) and categories for documenting outcomes of treatment (resolved, stable, improved, etc.).
2. It provides examples of using each outcome category in clinical cases, such as describing a pneumonia being resolved after antibiotic treatment or hypertension stabilized with medication.
3. The final outcomes discussed are worsened, failure, and expired, with examples of when a change in treatment is needed or a patient passes away during therapy.
Hak Cipta:
© All Rights Reserved
Format Tersedia
Unduh sebagai PPTX, PDF, TXT atau baca online dari Scribd
0 penilaian0% menganggap dokumen ini bermanfaat (0 suara)
9 tayangan13 halamanMembantu Pasien Dengan Gejala Dan Membawaa Produk Obat
Diunggah oleh
Misgi Candra Dasa1. The document discusses various frameworks for structuring patient consultations, including mnemonics to guide questioning (WHAM, ASMETHOD) and categories for documenting outcomes of treatment (resolved, stable, improved, etc.).
2. It provides examples of using each outcome category in clinical cases, such as describing a pneumonia being resolved after antibiotic treatment or hypertension stabilized with medication.
3. The final outcomes discussed are worsened, failure, and expired, with examples of when a change in treatment is needed or a patient passes away during therapy.
Hak Cipta:
© All Rights Reserved
Format Tersedia
Unduh sebagai PPTX, PDF, TXT atau baca online dari Scribd
Anda di halaman 1dari 13
Membantu pasien dengan gejala
dan membawa produk obat dalam
swamedikasi
Responding to a request for help with
symptoms
• 1 Information gathering
• 2 Decision making
• 3 Treatment
• 4 Outcome
Responding to a request for a named
product
• an expert or a novice user
• The pharmacy patient medication records
(PMRs) are a source of back-up information
for regular customers
Structuring the consultation
• W – Who is the patient and what are the
symptoms?
• H – How long have the symptoms been
present?
• A – Action taken?
• M – Medication being taken?
The second mnemonic, ASMETHOD,
was developed by Derek
Balon, a community pharmacist in
London:
• A – Age and appearance
• S – Self or someone else
• M – Medication
• E – Extra medicines
• T – Time persisting
• H – History
• O – Other symptoms
• D – Danger symptoms.
Outcome
• Resolved
• The patient's desired goals of therapy have been successfully achieved,
and drug therapy can be discontinued. The use of the term resolved is
intended to represent a final positive patient outcome, and is most often
applicable to acute medical conditions or illnesses. The action taken, in
this case discontinuing the drug therapy, should be documented in your
patient's pharmaceutical care records along with the clinical and/or
laboratory evidence of the positive outcome.
• Example Consider the case of a successful treatment of a community
acquired pneumonia in a 53-year male patient with a 10-day course of oral
erythromycin therapy at a dosage of 500 mg four times each day. By the
end of the 10 days of antibiotics, the patient's temperature is back to
normal, he has stopped coughing, his white blood count is no longer
elevated, and the infiltrates originally seen on his chest x ray have cleared.
He does not require any further antibiotics past the original 10-day course
of treatment. No additional follow-up is needed as his pneumonia has
resolved.
• Stable
• The patient's goals of therapy have been achieved, and the same drug
therapy will be continued to optimally manage the patient's chronic
disease. This is most frequently the case when drug therapy is used to
treat or prevent a chronic medical condition or illness. In these cases,
stabilizing the patient's clinical condition and/or improving laboratory test
results were the predetermined desired goals.
• Example In order to stabilize a 63 year old female patient's blood pressure
within a desired range of 110–120/70–80 within 2 months the practitioner
initiates pharmacotherapy with 50 mg of hydrochlorothiazide every
morning, a sodium restricted diet, and a low impact exercise program. At
the 60-day follow-up evaluation, the patient's blood pressure was 112/80
and her hypertension was judged to be stable and no changes in
hydrochlorothiazide dosage regimen were made. The next follow-up
evaluation might be planned to occur in 90 days to reevaluate the
continued success of the entire care plan.
• Improved
• Measurable progress is being realized in achieving the patient's
goals of therapy. Goals have not been completely achieved at this
time; however, no changes in drug therapy will be implemented at
this time because more time will be required to observe the full
benefit from this drug regimen.
• Example Consider a 55-year-old male patient whose depressive
signs and symptoms such as loss of energy and disturbances in
sleep and eating patterns have improved following an initial 3
weeks of drug therapy with 100 mg daily of the antidepressant drug
sertraline (Zoloft). Although his depressed mood and ability to
concentrate have still not fully responded, no changes in his dosage
regimen will be instituted at this time. In this case, an additional
follow-up evaluation would be scheduled for 4 weeks.
• Partial Improvement
• The evaluation indicates that some positive progress is being made
in achieving the patient's goals of therapy, but adjustments in drug
therapy are necessary at this time in order to fully meet all of the
goals of therapy by the next scheduled follow-up evaluation.
• Example A 47-year-old female patient whose arthritic pain has
been somewhat relieved following 2 weeks of therapy with
ketoprofen (Orudis) 12.5 mg four times daily, desires additional
relief from her discomfort. The practitioner's evaluation indicates
that greater effectiveness might be realized by increasing the total
daily dosage of ketoprofen to 75 mg taken as 25 mg three times
daily. The next follow-up evaluation is scheduled to occur in two
more weeks to determine if this adjustment in the dosage regimen
of the nonsteroidal anti-inflammatory medication produces
continued and/or additional relief for the patient without
intolerable stomach irritation, headache, or fluid retention.
• Unimproved
• The practitioner's clinical evaluation is that, to date, little or no positive progress
has been made in achieving the patient's goals of therapy, but further
improvement is still anticipated given more time. Therefore, the patient's care plan
will not be altered at this time. Thus, the unimproved status evaluation is
dependent on the timing of the follow-up evaluation.
• Example An adult male patient who is allergic to penicillin is started on
erythromycin 250 mg orally four times a day for the treatment of a localized soft
tissue infection following a work-related injury to the right forearm. Twenty-four
hours after initiating erythromycin therapy the patient experiences some nausea
from the antibiotic, and the injured area on the arm is still inflamed and slightly
swollen. The practitioner reassures the patient about the nausea and provides him
with a suggestion as to how to minimize this undesirable side effect commonly
associated with erythromycin, and documents an evaluation of the current
effectiveness of therapy. The practitioner reports that although the arm is
unimproved at this early stage in therapy, no dosage changes are indicated, and
that 3–5 days would be an appropriate time to make another evaluation of the
potential effectiveness of the erythromycin therapy.
• Worsened
• The practitioner's evaluation describes a decline in the health of the patient
despite an adequate therapeutic trial using the best possible drug therapy for this
individual. Because the goals of therapy are not being achieved, changes in the
patient's drug therapies are necessary at this time. The drug dosage may need to
be increased and/or additive or synergistic drug therapies might need to be added.
A future follow-up evaluation should be planned to examine the status of the
patient's condition once the changes in the care plan have been instituted.
• Example A 17-year-old athlete whose elbow stiffness and muscle pain have
progressively become more bothersome over the past 4 days despite the use of
acetaminophen 325 mg three times each day and ice packs. This worsening
condition might call for increasing the acetaminophen dosage and/or adding a
topical analgesic such as capsicum. Two days after increasing the acetaminophen
dosage to 1000 mg three times a day and adding topical capsicum, the practitioner
would follow-up again to determine the effectiveness in reducing the pain and
stiffness in this varsity athlete.
• Failure
• The practitioner's evaluation indicates that the present care plan
and associated drug therapies have been given at adequate dosages
and for an adequate amount of time, yet they have failed to help
the patient achieve the goals of therapy. Therefore, the present
therapy should be discontinued and alternate pharmacotherapy
initiated. In these situations, the desired outcomes have not been
realized and the initial treatment is considered to have failed.
• Example A 37-year-old female patient whose symptoms of seasonal
allergic rhinitis have not improved with 2 weeks of
chlorpheniramine therapy at 24 mg per day. Therefore, it will be
discontinued, and new drug therapy initiated such as loratadine
(Claritin) 10 mg daily. The next follow-up evaluation is planned in 5
days to examine the effectiveness of loratadine in controlling the
patient's symptoms of rhinitis.
• Expired
• The fact that the patient dies while receiving
drug therapy is documented in the
pharmaceutical care record. Any important
observations about contributing factors,
especially if they are drug-related, should be
noted
Anda mungkin juga menyukai
- Practical Insulin: A Handbook for Prescribing ProvidersDari EverandPractical Insulin: A Handbook for Prescribing ProvidersPenilaian: 5 dari 5 bintang5/5 (2)
- Drug Related ProblemDokumen34 halamanDrug Related ProblemERONADIAULFAH SUGITOBelum ada peringkat
- Pharmacoepidemiology, Pharmacoeconomics,PharmacovigilanceDari EverandPharmacoepidemiology, Pharmacoeconomics,PharmacovigilancePenilaian: 3 dari 5 bintang3/5 (1)
- Rational Use of Drugs-IDokumen38 halamanRational Use of Drugs-IUmair Mazhar100% (1)
- PDIS - Calculation of Medication DosesDokumen41 halamanPDIS - Calculation of Medication DosesMark Angelo JaurigueBelum ada peringkat
- Clinical MidDokumen13 halamanClinical MidUmair MazharBelum ada peringkat
- PharmacotherapyDokumen42 halamanPharmacotherapykhalid a.qazi100% (1)
- Myocardial InfarctionDokumen5 halamanMyocardial InfarctionDharline Abbygale Garvida AgullanaBelum ada peringkat
- Pharmaceutical and Clinical CalculationDokumen108 halamanPharmaceutical and Clinical CalculationAsh MBelum ada peringkat
- Acute Exacerbation of AsthmaDokumen28 halamanAcute Exacerbation of AsthmaMike singhBelum ada peringkat
- Calculation of Doses PT FactorsDokumen47 halamanCalculation of Doses PT Factorsmtlqhsn78Belum ada peringkat
- ComplianceDokumen13 halamanCompliancextremist2001Belum ada peringkat
- MedicationReview PracticeGuide2011Dokumen29 halamanMedicationReview PracticeGuide2011Yusnia Gulfa MaharaniBelum ada peringkat
- Causality Assessment of ADRsDokumen45 halamanCausality Assessment of ADRsKrupasagar Pn PalegarBelum ada peringkat
- Adverse Drug Reaction 1Dokumen48 halamanAdverse Drug Reaction 1Ankita PandaaBelum ada peringkat
- 02-Pharmaceutical Care ProcessDokumen42 halaman02-Pharmaceutical Care ProcessBalsam Zahi Al-Hasan100% (1)
- Medspan's Pharmacy Guide For OSCEDokumen8 halamanMedspan's Pharmacy Guide For OSCEDeviselvamBelum ada peringkat
- 1215 LHCC LA - CP.MP.34 Hyperemesis Gravidarum TreatmentDokumen9 halaman1215 LHCC LA - CP.MP.34 Hyperemesis Gravidarum TreatmentSatriyo Krisna PalgunoBelum ada peringkat
- Application of PK in Clinical SitutionDokumen42 halamanApplication of PK in Clinical Situtionsafia mehmood100% (1)
- Pharmaceutical CareDokumen26 halamanPharmaceutical CareNuha AgabnaBelum ada peringkat
- Prescription and AbbreviationDokumen54 halamanPrescription and Abbreviationsanjeev khanalBelum ada peringkat
- Treatment of TB in Adults: by Dr. Irfhan Ali Hyder AliDokumen45 halamanTreatment of TB in Adults: by Dr. Irfhan Ali Hyder AliInspireGutsBelum ada peringkat
- Power Point Treatment of Functional Dyspepsia With SertralineDokumen26 halamanPower Point Treatment of Functional Dyspepsia With SertralineRadias ZasraBelum ada peringkat
- UNIT4 Clinical PharmacyDokumen21 halamanUNIT4 Clinical PharmacyIsha AgarwalBelum ada peringkat
- Olanzapine For Nausea and VomitingDokumen42 halamanOlanzapine For Nausea and Vomitingsitiradziah subariBelum ada peringkat
- Crash Course New 1Dokumen416 halamanCrash Course New 1Today ViralBelum ada peringkat
- Care Plan 2Dokumen11 halamanCare Plan 2api-28474004567% (3)
- Nursing-Process-Focus-Drug-Study-Template Special AreaDokumen8 halamanNursing-Process-Focus-Drug-Study-Template Special AreaRose RanadaBelum ada peringkat
- Pharmaceutical Care PlanDokumen19 halamanPharmaceutical Care PlanDaenica Lorraine Abella SebastianBelum ada peringkat
- Complete Clinical PharmacyDokumen219 halamanComplete Clinical PharmacyCharles AbagonBelum ada peringkat
- Asthma Case Study Answers 20jan 202011 Web Module2Dokumen7 halamanAsthma Case Study Answers 20jan 202011 Web Module2Clarise Barcenal Briones100% (1)
- Screening Phase Up To 6 Weeks To Determine Study Eligibility. Open-Label Phase (Baseline To Visit OL22)Dokumen16 halamanScreening Phase Up To 6 Weeks To Determine Study Eligibility. Open-Label Phase (Baseline To Visit OL22)gemmaBelum ada peringkat
- Modern Dispensing AspectsDokumen36 halamanModern Dispensing AspectsHashim MohammedBelum ada peringkat
- Compilation of QuizzesDokumen10 halamanCompilation of QuizzesElesis samaBelum ada peringkat
- Rational Prescribing & Prescription Writing: IntroductionDokumen3 halamanRational Prescribing & Prescription Writing: IntroductionAnmol KudalBelum ada peringkat
- Ketamine, Originally Approved As An Anesthetic Drug, Is Gaining Ground As An Intervention For PatientsDokumen7 halamanKetamine, Originally Approved As An Anesthetic Drug, Is Gaining Ground As An Intervention For PatientsBabak AsliBelum ada peringkat
- NSRG 258 Principles of NursingDokumen11 halamanNSRG 258 Principles of NursingMayaka AmosBelum ada peringkat
- Nursing Care Plan: Assessment Nursing Diagnosis Analysis / Inference Planning Intervention / Rationale EvaluationDokumen4 halamanNursing Care Plan: Assessment Nursing Diagnosis Analysis / Inference Planning Intervention / Rationale EvaluationMon ManguilinBelum ada peringkat
- Publikasj JurnalDokumen6 halamanPublikasj JurnalFebrian StoreBelum ada peringkat
- NoncomplianceDokumen3 halamanNoncomplianceChristy BerryBelum ada peringkat
- Nursing Care Plan Cues Nursing Diagnosis Objectives Interventions Rationale Evaluation Short Term IndependentDokumen3 halamanNursing Care Plan Cues Nursing Diagnosis Objectives Interventions Rationale Evaluation Short Term IndependentChristy Berry100% (1)
- Three Component Model For Depression: Omer Zulfiqar MsiiiDokumen30 halamanThree Component Model For Depression: Omer Zulfiqar MsiiiozulfiqaBelum ada peringkat
- Chapter 001Dokumen8 halamanChapter 001Lisa SzyszkaBelum ada peringkat
- Drug Related ProblemsDokumen25 halamanDrug Related ProblemsChristine GanBelum ada peringkat
- A Guide To Patient Medication Review: September 2003Dokumen33 halamanA Guide To Patient Medication Review: September 2003Muhamad GunturBelum ada peringkat
- Neuropathic Pain TreatmentDokumen8 halamanNeuropathic Pain TreatmentIrimes MariaBelum ada peringkat
- Therapeutics Process: P-Drugs & P-TreatmentDokumen35 halamanTherapeutics Process: P-Drugs & P-TreatmentdesyisrooBelum ada peringkat
- Nursing Process in Administering MedicationsDokumen37 halamanNursing Process in Administering MedicationsLady Mae RamosBelum ada peringkat
- Jurnal B.ing Kelompok 3Dokumen37 halamanJurnal B.ing Kelompok 3Tata Dimas Al HaqBelum ada peringkat
- NCP Midterm Uncontrolled DMDokumen12 halamanNCP Midterm Uncontrolled DMYlron John Tapar100% (1)
- Lecture 2 Prescribing-1Dokumen21 halamanLecture 2 Prescribing-1Sante MunguyaBelum ada peringkat
- Therapeutical ProcessDokumen33 halamanTherapeutical ProcessecyzsiemoBelum ada peringkat
- MH Shared Care Guidelines For Prescribing ValproateDokumen5 halamanMH Shared Care Guidelines For Prescribing ValproateDr. Nivas SaminathanBelum ada peringkat
- Gradual Dose Reduction ScheduleDokumen5 halamanGradual Dose Reduction ScheduleAhmad Mujahid Huzaidi100% (1)
- Chest Suppl 22sDokumen17 halamanChest Suppl 22sMoisés PonceBelum ada peringkat
- Prescription - Writing PartDokumen38 halamanPrescription - Writing PartJnanesh PuniBelum ada peringkat
- Pediatric Health Nursing Unit-Iii Pharmacological Care Aspects While Dealing With Pediatric PatientsDokumen107 halamanPediatric Health Nursing Unit-Iii Pharmacological Care Aspects While Dealing With Pediatric PatientsPriya bhatti0% (1)
- NCP MiDokumen8 halamanNCP MiPitaca Madiam Annabehl PaulBelum ada peringkat
- 2.mood Disorder TreatmentDokumen56 halaman2.mood Disorder TreatmentREDEEM NBelum ada peringkat
- Part XI - NCPDokumen6 halamanPart XI - NCPjeslergarciachioBelum ada peringkat
- Health Promotion: Didik Setiawan, PHD., AptDokumen17 halamanHealth Promotion: Didik Setiawan, PHD., AptMisgi Candra DasaBelum ada peringkat
- Drug Induced DiseaseDokumen19 halamanDrug Induced DiseaseMisgi Candra DasaBelum ada peringkat
- Basic Principles of Epidemiology: Didik Setiawan, PHD., AptDokumen28 halamanBasic Principles of Epidemiology: Didik Setiawan, PHD., AptMisgi Candra DasaBelum ada peringkat
- Logo ApotekDokumen1 halamanLogo ApotekMisgi Candra DasaBelum ada peringkat
- Health Promotion: Didik Setiawan, PHD., AptDokumen17 halamanHealth Promotion: Didik Setiawan, PHD., AptMisgi Candra DasaBelum ada peringkat
- Presenting ResultsDokumen10 halamanPresenting ResultsMisgi Candra DasaBelum ada peringkat
- HHHHHHDokumen6 halamanHHHHHHMisgi Candra DasaBelum ada peringkat
- Usulan Program Kreativitas Mahasiswa: Frugie Momy)Dokumen8 halamanUsulan Program Kreativitas Mahasiswa: Frugie Momy)Misgi Candra DasaBelum ada peringkat
- Usulan Program Kreativitas Mahasiswa: Frugie Momy)Dokumen8 halamanUsulan Program Kreativitas Mahasiswa: Frugie Momy)Misgi Candra DasaBelum ada peringkat
- A National Assessment of Warfarin Anticoagulation Therapy ForDokumen21 halamanA National Assessment of Warfarin Anticoagulation Therapy ForMisgi Candra DasaBelum ada peringkat
- Chord PhotographDokumen1 halamanChord PhotographMisgi Candra DasaBelum ada peringkat
- ZometaDokumen6 halamanZometaMisgi Candra DasaBelum ada peringkat
- ZometaDokumen6 halamanZometaMisgi Candra DasaBelum ada peringkat
- Product Monograph - Zoledronic Acid For Injection ConcentrateDokumen58 halamanProduct Monograph - Zoledronic Acid For Injection ConcentrateMisgi Candra DasaBelum ada peringkat
- ZometaDokumen6 halamanZometaMisgi Candra DasaBelum ada peringkat
- Antihistamin PDFDokumen7 halamanAntihistamin PDFKarina Mega W100% (1)
- Over The Counter (OTC) Product List: Aetna Better Health®Dokumen5 halamanOver The Counter (OTC) Product List: Aetna Better Health®sarath chandraBelum ada peringkat
- Under Supervision of Dr. Ommia AliDokumen15 halamanUnder Supervision of Dr. Ommia AliAbdelrhman AboodaBelum ada peringkat
- Use and Safety Antihistamine For ChildrenDokumen10 halamanUse and Safety Antihistamine For Childrenbudianto_sigalingginBelum ada peringkat
- OTC Drug ListDokumen8 halamanOTC Drug ListcfgvhBelum ada peringkat
- FormularyDokumen29 halamanFormularykgnmatinBelum ada peringkat
- AntihistaminesDokumen24 halamanAntihistaminesWulan YuwitaBelum ada peringkat
- Respiratory and Cardiovascular Drugs QuestionsDokumen11 halamanRespiratory and Cardiovascular Drugs QuestionsMaria Chrislyn Marcos GenorgaBelum ada peringkat
- Over-The-Counter Medications in PregnancyDokumen8 halamanOver-The-Counter Medications in PregnancyKenef CheungBelum ada peringkat
- MGDokumen12 halamanMGelektron2010Belum ada peringkat
- AutacoidsDokumen8 halamanAutacoidsDeity CelleBelum ada peringkat
- Asthma in PregnancyDokumen20 halamanAsthma in PregnancyKelly Posadas-MesinaBelum ada peringkat
- Lippincott Illustrated Reviews (PDFDrive) - Pages-396Dokumen2 halamanLippincott Illustrated Reviews (PDFDrive) - Pages-396Eman ShalabyBelum ada peringkat
- Drug Benefit ListDokumen221 halamanDrug Benefit ListPharmaruthiBelum ada peringkat
- Interaksi Obat by MEDSCAPEDokumen4 halamanInteraksi Obat by MEDSCAPENila Permata Sari S.Si,AptBelum ada peringkat
- Effect of H1 Induced in Patients With Chronic Cough: Loratadine, Antihistamine, Cough Non-AsthmaticDokumen5 halamanEffect of H1 Induced in Patients With Chronic Cough: Loratadine, Antihistamine, Cough Non-AsthmaticFahmi PratamaBelum ada peringkat
- New Medicines On The Market: UK Medicines Information Pharmacists GroupDokumen6 halamanNew Medicines On The Market: UK Medicines Information Pharmacists GroupMohamed Talaat100% (1)
- AntihistaminesDokumen83 halamanAntihistaminesKishore ChandkiBelum ada peringkat
- Allergy MedicationsDokumen2 halamanAllergy Medicationsbarney_bestBelum ada peringkat
- Desloratadine - A New, Nonsedating, Oral AntihistamineDokumen12 halamanDesloratadine - A New, Nonsedating, Oral AntihistamineAnonymous so6ZnlKywBelum ada peringkat
- AntihistaminesDokumen4 halamanAntihistaminessharvabhasin0% (1)
- OtcDokumen10 halamanOtcJames PerianayagamBelum ada peringkat
- Pharmacology For Nursing - Section I-UNit 1 - Introduction To Nursing PharmacologyCh 1&2-Dr Hanan Youssef - 40-41-1Dokumen124 halamanPharmacology For Nursing - Section I-UNit 1 - Introduction To Nursing PharmacologyCh 1&2-Dr Hanan Youssef - 40-41-1Jnm NenBelum ada peringkat
- Drug CompilationDokumen39 halamanDrug CompilationANa AntonioBelum ada peringkat
- Clarinase Repetabs Leaflet (Eng) - CCDS 122013-2014-06-26Dokumen2 halamanClarinase Repetabs Leaflet (Eng) - CCDS 122013-2014-06-26Andrew LienataBelum ada peringkat
- Restructuring: Business Strategy Project ReportDokumen34 halamanRestructuring: Business Strategy Project ReportefgkBelum ada peringkat
- Preferred Drug ListDokumen2 halamanPreferred Drug ListRamBelum ada peringkat
- 3 AntihistamineDokumen46 halaman3 Antihistaminepranay shettigarBelum ada peringkat
- Allergic PDFDokumen17 halamanAllergic PDFSiska HarapanBelum ada peringkat
- Aerius Syrup PIDokumen9 halamanAerius Syrup PITerrence LiBelum ada peringkat
- PH Info ExamDokumen44 halamanPH Info ExamANa AntonioBelum ada peringkat