Poly Neuropathy
Diunggah oleh
Doha Ebed0 penilaian0% menganggap dokumen ini bermanfaat (0 suara)
13 tayangan16 halamanpolyneuropathy causes investigations
Hak Cipta
© © All Rights Reserved
Format Tersedia
PPTX, PDF, TXT atau baca online dari Scribd
Bagikan dokumen Ini
Apakah menurut Anda dokumen ini bermanfaat?
Apakah konten ini tidak pantas?
Laporkan Dokumen Inipolyneuropathy causes investigations
Hak Cipta:
© All Rights Reserved
Format Tersedia
Unduh sebagai PPTX, PDF, TXT atau baca online dari Scribd
0 penilaian0% menganggap dokumen ini bermanfaat (0 suara)
13 tayangan16 halamanPoly Neuropathy
Diunggah oleh
Doha Ebedpolyneuropathy causes investigations
Hak Cipta:
© All Rights Reserved
Format Tersedia
Unduh sebagai PPTX, PDF, TXT atau baca online dari Scribd
Anda di halaman 1dari 16
Polyneuropathies can be classified
by:
• Modality affected: sensory, motor, sensorimotor,
autonomic
• Fiber type affected:
– large fiber (proprioception/vibration)
– versus small fiber (pain/temperature)
Clinically, large-fiber neuropathies can be distinguished from small-
fiber neuropathies during neurologic testing: large fibers carry
sensation for vibration and proprioception, while small fibers carry
sensation for pain and temperature. Sensation for light touch is
carried by both large and small nerve fibers.
• Pathophysiology: axonal versus demyelinating
• Categorized by either clinical symptom distribution (length
dependent, length independent, or multifocal)
length-dependent peripheral
neuropathy
• The most common pattern of clinical involvement is that of a
length-dependent peripheral neuropathy. This form of neuropathy
is symmetric, and symptoms begin in the longest nerves at their
terminals (ie, distal foot). Negative (lack of feeling) or positive
(prickling, tingling, burning) sensory symptoms usually precede
motor weakness. The symptoms ascend insidiously up the leg, with
hand symptoms often becoming evident around the time leg
symptoms approach the knee. Upper limb involvement may never
occur. Development of symptoms in the hands and feet at the same
time is atypical for a diabetic length-dependent neuropathy and
may indicate coexisting carpal tunnel syndrome.
• Proprioception is spared relative to other sensory modalities in mild
to moderate length dependent neuropathies and only becomes
affected as the neuropathy severity progresses
length-independent polyneuropathy
• Sensory and/or motor symptoms in a more
diffuse, length-independent pattern (ie, involving
both proximal and distal limbs) suggest a
polyradiculoneuropathy.
• Although these neuropathies may still be sensory
predominant motor manifestations are usually
more evident than in length-dependent
neuropathies. Reflexes can be useful in these
cases because they are globally reduced or
absent.
Multifocal neuropathy
• Rare patients present with multifocal clinical symptoms
(eg, a wrist drop, followed by a foot drop). As multifocal
processes progress, further neurologic deficits accrue, and
the process may begin to look more diffuse. Careful
history and examination are necessary to recognize these
multifocal neuropathies.
• Polyradiculoneuropathies and multifocal neuropathies
have a distinct differential diagnosis from that for length-
dependent neuropathies. Etiologies include sarcoidosis,
amyloidosis, and neoplastic, paraneoplastic, vasculitic,
infectious, and inflammatory immune-mediated causes
(such as chronic inflammatory demyelinating
polyradiculoneuropathy),
• Most recommendations for office screening for
neuropathy have utilized the following:
1. light touch perception to a 10-g Semmes-
Weinstein monofilament
2. vibration testing with a 128-Hz tuning fork
3. superficial pain (pinprick) perception testing
4. ankle deep tendon reflexes
• If single-modality screening is used, monofilament
light touch or vibration testing appears to be more
sensitive and specific than superficial pain
(pinprick) or ankle reflex testing
SYMPTOMS SUGGESTING PERIPHERAL
NEUROPATHY
• Sensory symptoms (eg, numbness,
tingling), or neuropathic (burning,
• stabbing, electrical) pain
• Motor weakness
• Autonomic symptoms (eg, early satiety,
impotence, orthostatic hypotension,
• sweat abnormalities),
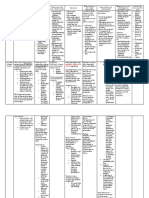
causes
• DM (but not IGT)
• Vitamin B12 deficiency can cause classic subacute combined
degeneration or an isolated peripheral neuropathy without central
nervous system involvement
• Dysproteinemias (amyloidosis, MM, MGUS, Cryoglobinemia
• Infections(HIV, Lyme)
• Vasculitis
• Celiac disease: small-bowel biopsy should be obtained before
attributing neuropathy to celiac disease
• Paraneoplastic
• Other nutritional deficiencies (Cupper, vitamin E)
• Toxic Neuropathies.
• Rarely hypothyroidism
• Hereditary Neuropathies
Investigations
• FBG, or HbA1c
• Vitamin B12 with methylmalonic acid
• serum protein immunofixation electrophoresis
• Complete blood cell count
• Renal function
• Liver function tests
• Erythrocyte sedimentation rate
• Thyroid stimulating hormone
• Screen for HIV, lyme disease
• Screen for celiac disease (Anti-tissue transglutaminase
antibodies
• Screen for autoimmune causes
Other Diagnostic Tests
Nerve Conduction Studies and
Electromyography.
• electromyography (EMG) and nerve conduction
studies (NCSs) are useful to
1. Confirm the suspected diagnosis
2. exclude mimickers (S1 radiculopathies in a patient with
foot symptoms or carpal tunnel syndrome in a patient
with hand paresthesias),
3. localize the process (length dependent, length
independent, multifocal),
4. confirm the modalities affected (sensory, motor),
5. define whether the neuropathy is secondary to axonal
loss, demyelination, or both
6. Define the severity of the neuropathy.
• Electromyography/NCSs assess the function and
integrity of large, myelinated A beta nerve
fibers. They do not assess small nerve fibers (C
fiber and small myelinated A delta). As such,
normal findings on EMG do not exclude a small-
fiber peripheral neuropathy (which clinically
presents with prominent pain, sensory loss, and
dysautonomia).
Test of Small Nerve Fiber Function.
• A number of tests can evaluate possible small-
fiber peripheral neuropathies
(autonomic reflex screen, testing of sweat
function, quantitative sensory testing, and
epidermal skin biopsy for nerve fiber density)
Diabetic radiculopathy
• Usually has subacute onset
• Mostly lumbosacral but less commonly
cervical or thoracic
Rare
• Copper deficiency can mimic vitamin B12
deficiency clinically (with a myelopathy and
sensory-predominant neuropathy) and should be
considered when patients have a history of
bariatric surgery or multiple nutritional
deficiencies or if high zinc exposure (nutritional
supplement or in some denture pastes) is
suspected.
• Vitamin E deficiency may be considered in patients
at risk for fat malabsorption.
Toxic Neuropathies
• Excessive, long-term alcohol
• Chemotherapy
• Phenytoin
• Nitrofurantoin
• INH
• Flagyl
• Linozolid
Hereditary Neuropathies
• Clinically, a hereditary neuropathy is suggested by an
insidious onset of symptoms with a slow progressive
course over years,
• distal-predominant motor greater than sensory
complaints, lack of positive sensory symptoms
(dysesthesias, burning),
• associated structural foot and ankle deformity (pes
cavus, hammertoes, and inverted champagne bottle
legs with very thin ankles),
• and a family history of neuropathy. It is common that
family members are unaware of a family history even
when one is present
Anda mungkin juga menyukai
- The Yellow House: A Memoir (2019 National Book Award Winner)Dari EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Penilaian: 4 dari 5 bintang4/5 (98)
- Third Nerve Palsy Analysis of 1400 Personally Examined InpatientsDokumen9 halamanThird Nerve Palsy Analysis of 1400 Personally Examined Inpatientstenthousand hoursBelum ada peringkat
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceDari EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RacePenilaian: 4 dari 5 bintang4/5 (895)
- Tli Terminal Latency Index KayDokumen5 halamanTli Terminal Latency Index KayAnonymous 9lmlWQoDm8Belum ada peringkat
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeDari EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifePenilaian: 4 dari 5 bintang4/5 (5794)
- Chemotherapy-Induced Peripheral NeuropathyDokumen22 halamanChemotherapy-Induced Peripheral Neuropathyapi-238658139Belum ada peringkat
- The Little Book of Hygge: Danish Secrets to Happy LivingDari EverandThe Little Book of Hygge: Danish Secrets to Happy LivingPenilaian: 3.5 dari 5 bintang3.5/5 (400)
- Lidocaine Infusion A Promising Therapeutic Approach For Chronic PainDokumen14 halamanLidocaine Infusion A Promising Therapeutic Approach For Chronic PaingabhekBelum ada peringkat
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaDari EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaPenilaian: 4.5 dari 5 bintang4.5/5 (266)
- Harden Bruehl 2005 Diagnostic Criteria The Statistical Derivation of The Four Criterion FactorDokumen15 halamanHarden Bruehl 2005 Diagnostic Criteria The Statistical Derivation of The Four Criterion FactorroooBelum ada peringkat
- Shoe Dog: A Memoir by the Creator of NikeDari EverandShoe Dog: A Memoir by the Creator of NikePenilaian: 4.5 dari 5 bintang4.5/5 (537)
- Prevention of Foot Ulcer 2020Dokumen22 halamanPrevention of Foot Ulcer 2020Devi SiswaniBelum ada peringkat
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureDari EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FuturePenilaian: 4.5 dari 5 bintang4.5/5 (474)
- 2 in 1 P5VS Guideline 2018 (3rd Ed.) PDFDokumen50 halaman2 in 1 P5VS Guideline 2018 (3rd Ed.) PDFAzian ZainalBelum ada peringkat
- Never Split the Difference: Negotiating As If Your Life Depended On ItDari EverandNever Split the Difference: Negotiating As If Your Life Depended On ItPenilaian: 4.5 dari 5 bintang4.5/5 (838)
- Lepra ReactionDokumen24 halamanLepra ReactionSWAPAN KUMAR SARKAR100% (2)
- Grit: The Power of Passion and PerseveranceDari EverandGrit: The Power of Passion and PerseverancePenilaian: 4 dari 5 bintang4/5 (588)
- Pain Assessment: The Fifth Vital Sign: Lesson Plan ForDokumen10 halamanPain Assessment: The Fifth Vital Sign: Lesson Plan ForfajaqaBelum ada peringkat
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryDari EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryPenilaian: 3.5 dari 5 bintang3.5/5 (231)
- 2022 Masingue P.Latour Rev Neurol Genetic Analysis in HereditaryDokumen20 halaman2022 Masingue P.Latour Rev Neurol Genetic Analysis in HereditaryLéo VidoniBelum ada peringkat
- CBT-Chronic Pain - Therapist - Manual PDFDokumen124 halamanCBT-Chronic Pain - Therapist - Manual PDFDee Kay100% (2)
- The Emperor of All Maladies: A Biography of CancerDari EverandThe Emperor of All Maladies: A Biography of CancerPenilaian: 4.5 dari 5 bintang4.5/5 (271)
- Key Answers Part 1 June 2019 PDFDokumen15 halamanKey Answers Part 1 June 2019 PDFNimer Abdelhadi AliBelum ada peringkat
- Anestesi - 02 Review UKMPPDDokumen87 halamanAnestesi - 02 Review UKMPPDNia UswantiBelum ada peringkat
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyDari EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyPenilaian: 3.5 dari 5 bintang3.5/5 (2259)
- 2021 American College of Rheumatology Vasculitis FoundationDokumen10 halaman2021 American College of Rheumatology Vasculitis FoundationVerónica Duménez JofréBelum ada peringkat
- On Fire: The (Burning) Case for a Green New DealDari EverandOn Fire: The (Burning) Case for a Green New DealPenilaian: 4 dari 5 bintang4/5 (73)
- Vibration DiseaseDokumen55 halamanVibration DiseaseVirgilioBelum ada peringkat
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersDari EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersPenilaian: 4.5 dari 5 bintang4.5/5 (344)
- Disorders of Optic Nerve and Visual Pathways: Ipek MidiDokumen24 halamanDisorders of Optic Nerve and Visual Pathways: Ipek MidiEcaterina ChiriacBelum ada peringkat
- Rise of ISIS: A Threat We Can't IgnoreDari EverandRise of ISIS: A Threat We Can't IgnorePenilaian: 3.5 dari 5 bintang3.5/5 (137)
- Analgesic Herbs Paper SWEETDokumen12 halamanAnalgesic Herbs Paper SWEETJames CookeBelum ada peringkat
- Team of Rivals: The Political Genius of Abraham LincolnDari EverandTeam of Rivals: The Political Genius of Abraham LincolnPenilaian: 4.5 dari 5 bintang4.5/5 (234)
- The Pathway: The Human Respiratory SystemDokumen25 halamanThe Pathway: The Human Respiratory SystemKenneth Decker PrietoBelum ada peringkat
- Approach To The Patient With Difficult in Walking (Hemiplegia)Dokumen78 halamanApproach To The Patient With Difficult in Walking (Hemiplegia)Ruby BhattyBelum ada peringkat
- Guillain-Barré SyndromeDokumen60 halamanGuillain-Barré SyndromekharaBelum ada peringkat
- The Unwinding: An Inner History of the New AmericaDari EverandThe Unwinding: An Inner History of the New AmericaPenilaian: 4 dari 5 bintang4/5 (45)
- Electroacupuncture: An Introduction and Its Use For Peripheral Facial ParalysisDokumen19 halamanElectroacupuncture: An Introduction and Its Use For Peripheral Facial ParalysisLuís CorreiaBelum ada peringkat
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreDari EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You ArePenilaian: 4 dari 5 bintang4/5 (1090)
- ETHAMBUTOLDokumen11 halamanETHAMBUTOLIrbasMantiniSyaifulBelum ada peringkat
- Differential Diagnosis of Cervicobrachial PainDokumen11 halamanDifferential Diagnosis of Cervicobrachial PainpuchioBelum ada peringkat
- Managing Your DiabetesDokumen34 halamanManaging Your DiabetesDeresse KebedeBelum ada peringkat
- 3rd Announcement PIN PERDOSSIDokumen34 halaman3rd Announcement PIN PERDOSSIAomc Pin PerdossiBelum ada peringkat
- Type of GaitsDokumen4 halamanType of GaitsSyimah UmarBelum ada peringkat
- ASSESSMENT OF PREVALENCE OF DIABETIC FOOT ULCER ANDASSOCIATED FACTORS AMONG DIABETIC PATIENT ATTENDING FHCSH DIABETIC CLINIC EditedDokumen31 halamanASSESSMENT OF PREVALENCE OF DIABETIC FOOT ULCER ANDASSOCIATED FACTORS AMONG DIABETIC PATIENT ATTENDING FHCSH DIABETIC CLINIC EditedAlex Tebkew100% (1)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)Dari EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Penilaian: 4.5 dari 5 bintang4.5/5 (121)
- Pain Terms: A Current List With Definitions and Notes On UsageDokumen9 halamanPain Terms: A Current List With Definitions and Notes On UsagealexandruBelum ada peringkat
- Diabetic Foot Case PresentationDokumen58 halamanDiabetic Foot Case PresentationMissoSandoqji100% (1)
- 00 - Nenoin Toolbox 1st Round of Assets - FinalDokumen21 halaman00 - Nenoin Toolbox 1st Round of Assets - FinalFakeGBelum ada peringkat
- Her Body and Other Parties: StoriesDari EverandHer Body and Other Parties: StoriesPenilaian: 4 dari 5 bintang4/5 (821)