NCP
Diunggah oleh
Jo Chiko FlorendoDeskripsi Asli:
Judul Asli
Hak Cipta
Format Tersedia
Bagikan dokumen Ini
Apakah menurut Anda dokumen ini bermanfaat?
Apakah konten ini tidak pantas?
Laporkan Dokumen IniHak Cipta:
Format Tersedia
NCP
Diunggah oleh
Jo Chiko FlorendoHak Cipta:
Format Tersedia
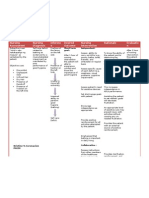
Nursing Problem with Cues Nursing Diagnosis with Objectives (SMART) Nursing Interventions Nursing Interventions Rationale Evaluation
Rationale
1. Abdominal pain Chronic Pain r/t physical Short-term: Independent: 1. Pain is not always present, but if Short-term:
response to disease After 2 hours of nursing 1. Noted reports of pain including location, duration, present should be compared with Partially met. There’s minimal
Subjective Data: interventions, patient will intensity and reviewed factors that alleviate or patient’s previous pain symptoms. This facial grimace, though abdominal
“I experience pain every 15-30 minutes for 10 seconds Rationale: verbalized decrease of pain aggravate pain. comparison may assist in diagnosis of guarding is still present patient
with a pain scale of 10/10.” as verbalized by the from 10 to 7, absence of facial etiology of bleeding and development of verbalized decrease of pain from
patient Pain is highly subjective state in grimace, will demonstrate complications. 10/10 to 8/10.
which a variety of unpleasant relapse body posture and be 2. Note nonverbal pain cues, e.g., restlessness,
Objective Data: sensations and a wide range of able to rest appropriately. reluctance to move, abdominal guarding, tachycardia, 2. Nonverbal cues may be both
Vital signs: T – 38.7 °C, RR – 22 bpm, HR – 110 distressing factors may be diaphoresis. Investigate discrepancies between verbal physiologic and psychological and may
bpm experienced by the sufferer. Long-term: and nonverbal cues. be used in conjunction with verbal cues
Facial grimace Pain may be symptom of injury After the 8-hour shift, patient to evaluate extent/severity of the
Abdominal guarding or illness. will verbalized tolerance to 3. Provide frequent oral care and comfort measures, problem.
Body rigidity pain as evidenced by improved e.g., back rub, position change. Long-term:
Ref: (Doenges, Moorhouse, & sleeping pattern, relapse body 3. Halitosis from stagnant oral secretions Goal met. After an 8-hour
Murr, 2013) posture, normal vital signs, and is unappetizing and can aggravate intervention patient verbalized
absence of facial grimace. 4. Provided and implemented prescribed dietary nausea. Gingivitis and dental problems improved sleeping pattern, vital
modifications. may arise. signs in normal range, and absence
of facial grimace
5. Administer medications, as indicated, e.g.: 4. Patient may be NPO initially. When
Antacids; oral intake is allowed, food choices will
depend on the diagnosis and the etiology
HEALTH TEACHING of the bleeding.
- Provide anticipatory guidance to client with
condition in which pain is common and educate about 5. Decreases gastric acidity by absorption
when, where, and how to seek intervention or or by chemical neutralization. Evaluation
treatments. type of antacid in regard to total health
-Assist client and SO(s) to learn how to heal by picture, e.g., sodium restriction
developing sense of internal control, by being
responsible for own treatment, and by obtaining the Ref: (Doenges, Moorhouse, & Murr,
information and tools to accomplish this. 2013)
Discuss potential for developmental delays in child
with chronic pain. Identify current level of function
and review appropriate expectations for individual
child.
Ref: (Doenges, Moorhouse, & Murr, 2013)
Nursing Problem with Cues Nursing Diagnosis with Objectives (SMART) Nursing Interventions Nursing Interventions Rationale Evaluation
Rationale
2. Weight loss Independent: 1. Provides rest for GI tract during Short-term:
Impaired Balance Nutrition Short-term: 1. Maintain patency of jejunostomy tube. acute postoperative phase until Goal met. Patient verbalized
Subjective Data: less than Body Within 5 hours of nursing return of normal function. understanding of functional
“I think, I lost half of my weight” as verbalized Requirements r/t change in interventions, patient will changes.
by the patient digestive verbalize understanding of 2. Will be bloody for first 12 hours,
process/absorption of functional changes. 2. Note character and amount of gastric and then should clear/ turn greenish.
nutrients drainage. Continued recurrent bleeding
Objective Data: Long-term: suggests complications. Decline in
Weight: Rationale: After 1 week of nursing output may reflect progression of Long-term:
Prior to admission – 60 kg Adequate nutrition is interventions, patient will fluid through the GI tract, suggesting Goal not met. The patient
April 30, 2018 – 30 kg necessary to meet the be able to demonstrate 3. Monitor tolerance to fluid and food intake, return of function. maintained her weight.
Prominent bones body’s demands. Nutritional progressive weight gain of 2 noting abdominal distension, reports of
BMI: 14, underweight status can be affected by kl per week. increased pain/ cramping, nausea/ vomiting. 3. Complications of paralytic ileus,
Decreased creatinine 33 umol\L disease. obstruction, delayed gastric
(4-7-19) emptying, and gastric dilation may
Ref: (Doenges, Moorhouse, Collaborative: occur, possibly requiring reinsertion
& Murr, 2013) 4. Administer IV fluids, TPN, and lipids as of NG tube.
indicated.
4. Meets fluid/nutritional needs
5. Progress diet as tolerated, advancing from until oral intake can be resumed.
clear liquid to bland diet with several small
feedings. 5. Usually NG tube is clamped for
specified periods of time when
HEALTH TEACHING peristalsis returns, to determine
- Emphasizes importance of well-balanced, tolerance. After NG tube is removed,
nutritious intake. Provide information regarding intake is advanced gradually to
individual nutritional needs and ways to meet prevent gastric irritation/distension.
these needs within financial constraints.
-Provide positive regard, love, and acknowledge Ref: (Doenges, Moorhouse, & Murr,
of “voice within” guiding client with eating 2013)
disorder.
-Develop consistent, realistic weight goal with
client.
(Doenges, Moorhouse, & Murr, 2013)
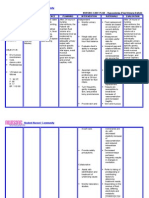
Nursing Problem with Cues Nursing Diagnosis with Objectives (SMART) Nursing Interventions Nursing Interventions Rationale Evaluation
Rationale
3. Presence of Jejunostomy tube (Jtube) Disturbed body image Short-term: Independent: 1. Provides information about Short-term:
related to insertion of After 2 hours of nursing 1. Ascertain whether counselling was initiated patient’s / SO’s level of knowledge Goal met. After 2 hour of
Subjective cues: Jejunostomy tube intervention, patient will when the possibility and/ or necessity of ostomy about individual situation and nursing intervention, patient
“I feel shy and less confident now that I have a verbalize feeling about the was first discussed. process of acceptance. verbalized feelings about the
tube in my stomach.” as verbalized by the Rationale: stoma and will demonstrate incision and demonstrated
patient A disturbance or alternation beginning acceptance by 2. Encourage patient/ SO to verbalize feelings 2. Helps the patient to realize that acceptance by participating in
in the attitude of person has viewing stoma and regarding the ostomy. Acknowledge normality of feelings are not unusual and that self-care and viewing stoma
Objective cues: about the actual or participating in self-care. feelings of anger, depression, and grief over loss. feeling guilty about them is not
Presence of Jejunostomy tube (Jtube) perceived structure or Discuss daily “ups and downs” that can occur. necessary/ helpful. Patient needs to
functions of all part of the recognize feelings before they can
body. This attitude is Long-term: be dealt with effectively.
dynamic and altered After 5 hours of nursing 3. Provide opportunity for patient to deal with
through interaction with intervention, patient will ostomy through participation in self-care. 3. Independence in self-care helps to Long-term: Goal met. After 5
other persons and situations Verbalize acceptance of the improve self-confidence and hours of intervention, patient
and is influenced by age and situation, incorporating acceptance of situation. verbalized acceptance to
developmental level. change into self-concept situation.
without negative self- 4. Maintain positive approach during care 4. Assists patients/ SO to accept
Ref: (Doenges, Moorhouse, esteem. activities, avoiding expressions of disdain or body changes and feel all right about
& Murr, 2013) revulsion. Do not take angry expressions self. Anger is most often directed at
personal the situation and lack of control
individual has over what has
happened (powerlessness), not with
the individual caregiver.
5. Note behaviours of withdrawal, increased 5. Suggestive of problems in
dependency, manipulation, or non-involvement adjustment that may require
in care. further evaluation and more
Health Teaching extensive therapy.
Ref: (Doenges, Moorhouse, & Murr, 2013)
Ref: (Doenges, Moorhouse, & Murr,
2013)
Nursing Problem with Cues Nursing Diagnosis with Objectives (SMART) Nursing Interventions Nursing Interventions Rationale Evaluation
Rationale
4. Anxiety Anxiety related to change in Short-term: Independent: 1. May indicative of the degree of Short term:
health status After 1 hour of nursing 1. Monitor physiologic responses, e.g., fear patient is experiencing but may Goal met
Subjective Data: intervention, patient will headache, dizziness, tingling sensations. also be related to physical After an hour of intervention,
”I’m scared of what will happen to me in the Rationale: verbalize appropriate range condition/shock state. patient verbalized appropriate
future.” as verbalized by the patient A vague uneasy feeling of of feelings. She will appear range of feeling. She was
discomfort or dread relaxed and report anxiety 2. Establishes a therapeutic relaxed and reported reduced
accompanied by an is reduced to manageable 2. Encourage verbalization of concerns. Assist relationship. Assists the patient in anxiety.
Objective Data: automatic response; the level. patient in expressing feelings by active listening. dealing with feelings and provides
Restlessness source often non-specific or opportunity to clarify
Irritability unknown to the individual; Long-tern: misconceptions.
HR – 110 bpm a feeling of apprehension After 8-hour shift, patient
Diaphoresis caused by anticipation of will discussed 3. When patient is expressing own Long term:
Increased tension danger. It is an altering fears/concerns recognizing 3. Acknowledge that this is a fearful situation fear, the validation that these Goal met.
signal that warns of healthy vs. unhealthy fears. and that others have expressed similar fears. feelings are normal can help patient After the nursing
impending danger and Patient will demonstrate to feel less isolated. Intervention
enables the individual to problem-solving and demonstrated problem
take measures to deal with effective use of resources. 4. Helps reduce fear of going, solving and effective
threat. through a frightening experience and effective use of
4. Encourage SO to stay with patient as able. alone. resources.
Ref: (Doenges, Moorhouse, Respond to call signal promptly. Use touch and
& Murr, 2013) eye contact as appropriate. 5. Removing patient from
outside stressors promotes
5. Provide a calm, restful environment. relaxation, may enhance
coping skills.
Ref: (Doenges, Moorhouse, & Murr, 2013)
Ref: (Doenges, Moorhouse, & Murr,
2013)
Nursing Problem with Cues Nursing Diagnosis with Objectives (SMART) Nursing Interventions Nursing Interventions Rationale Evaluation
Rationale
5. Knowledge deficit Risk for infection Short-term: Independent: Short-term:
transmission r/t lack of After an hour of 1. Educate the mother of the patient about Goal met. Mother of the
Subjective Data: knowledge reducing the intervention to the mother the importance of letting the patient patient understood that the
“My daughter does not know she has HIV” as risk of transmitting HIV of the patient, she will know about HIV. patient has to know he
verbalized by the patient’s mother. understand the importance condition but asked for more
Rationale: of letting the patient know 2. Identify susceptible Individuals 2. Contested susceptible time and wants to do it alone
Objective Data: HIV can be transmitted via of her condition. individuals to be tested for HIV,
the exchange of body fluids - Homosexual practices Some high risk behaviours can be
from one infected Long-term: - Bisexual practices eliminated. A professional in high- Long-term:
individuals to a healthy After 5 hours of nursing - IV/Intranasal/ Intradermal drug users risk situations must practice Goal not met. Patient’s
person, ignorance to how intervention, the patient - Health care workers universal precaution. mother did not tell the
HIV is transmitted and will know her condition - First responders (police, rescue workers, patient her condition.
acquired s detrimental to and will begin to accept it ambulance, fire-fighters).
HIV prevention efforts. by verbalizing her
understanding to HIV and
Ref: (Hong, Daria, […] and will comply to the
Mwamburi, Knowledge of therapies ordered by the 3. Discuss the mode of transmission of the 3. HIV is transmitted by sexual
HIV transmission and physician virus. contact, by contact with infected
associated factors, Journal - Unprotected vaginal, anal, or oral sex with blood, body fluid and blood
of AIDS & Clinical research, infected hosts or infected sex paraphernalia. products, and prenatally.
- Unprotected sex with infected person.
- Breastfeeding, perinatal transmission.
4. Reduce the risk of transmission of HIV. 4. The risk of developing sexually
Explain low-risk sexual m behaviours : transmitted infections is prevented
- Mutual masturbation with abstinence. Activities that do
- Massage not include penile, vaginal, anal, or
Vaginal intercourse with condom. oral contact carry low or no risk.
Transmission is reduced by condom
we and limiting having multiple
partners.
Nursing Problem with Cues Nursing Diagnosis with Objectives (SMART) Nursing Interventions Nursing Interventions Rationale Evaluation
Rationale
5. Provide Facts to dispel myths regarding 5. Dispelling myths and correcting
HIV transmission. misinformation can reduce
- The AIDS virus is not transmitted by anxiety and allow others to
mosquitoes, swimming pools, clothes, eating interact more normally with the
utensils, telephones, toilet seats, or close client.
contact.
- Saliva, sweat, tears, urine, and feces do not
transmit HIV.
6. Initiate Health Teaching and Referrals as 6. Protocols for exposure to body
Indicated fluids possibly contaminated with
-Emphasize the need to be careful when HIV are available in all health care
choosing sex partners (past sexual partners, facilities.
experimentation with drugs).
-Provide the community and the schools Ref: (Doenges, Moorhouse, &
with facts regarding AIDS transmission, and Murr, 2013)
dispels myths.
Health Teaching
Promote wellness
(teaching/Discharge Consideration)
- Review individual nutritional needs,
appropriate exercise program, and need for
rest
-Discuss the role of smoking in respiratory
infections.
-Provide information and involve in
appropriate community and national
education programs to increase awareness
of and prevention of communicable
diseases.
(Doenges, Moorhouse, & Murr, 2013)
Anda mungkin juga menyukai
- Acute PainDokumen5 halamanAcute PainJan Heartini SalvadorBelum ada peringkat
- Cutaneous Anthrax Nursing Care PlanDokumen2 halamanCutaneous Anthrax Nursing Care PlanYayin Pestaño100% (1)
- "Hindi Ko Kayo Masyadong Marinig Sa Kanang Tenga Ko, Pwede Bang Sa Kaliwang Side Ko Kayo Magsalita?" As Verbalized by The PatientDokumen2 halaman"Hindi Ko Kayo Masyadong Marinig Sa Kanang Tenga Ko, Pwede Bang Sa Kaliwang Side Ko Kayo Magsalita?" As Verbalized by The PatientMussaib Mushtaq100% (1)
- GENERAL SANTOS DOCTORS’ MEDICAL SCHOOL FOUNDATION NURSING CARE PLANDokumen4 halamanGENERAL SANTOS DOCTORS’ MEDICAL SCHOOL FOUNDATION NURSING CARE PLANFran LanBelum ada peringkat
- NCPDokumen3 halamanNCPbjhilarioBelum ada peringkat
- Nursing Care Plan HemorroidsDokumen2 halamanNursing Care Plan HemorroidsCaryl CagampangBelum ada peringkat
- NCP PTBDokumen2 halamanNCP PTBMack Jhed AnarconBelum ada peringkat
- NURSING-CARE-PLAN-Lung-Cancerxxx 1Dokumen3 halamanNURSING-CARE-PLAN-Lung-Cancerxxx 1Caroline ChaBelum ada peringkat
- Imbalance Nutrition Lass Than Body Requirements Related To Loss of Appetite Due To Aging 2Dokumen2 halamanImbalance Nutrition Lass Than Body Requirements Related To Loss of Appetite Due To Aging 2Senyorita KHaye100% (1)
- NCPDokumen4 halamanNCPMichelleBelum ada peringkat
- Nursing Care Plan: IndependentDokumen2 halamanNursing Care Plan: IndependentAdhaBelum ada peringkat
- ASSESSMENT HEALTH NURSING INTERVENTION EVALUATIONDokumen3 halamanASSESSMENT HEALTH NURSING INTERVENTION EVALUATIONtflorenzBelum ada peringkat
- Improving Neonatal Tissue Perfusion for SepsisDokumen2 halamanImproving Neonatal Tissue Perfusion for SepsisNiña Montejo Ealdama100% (1)
- NCP Self EsteemDokumen3 halamanNCP Self EsteemAlfadz AsakilBelum ada peringkat
- NCP CarpioDokumen7 halamanNCP CarpioFrancis Polycarp DiazBelum ada peringkat
- Nursing Care Plan for a Patient with JaundiceDokumen2 halamanNursing Care Plan for a Patient with JaundiceRachel Boton100% (2)
- NCP 2Dokumen3 halamanNCP 2klawdin100% (1)
- Hypertonic SolutionsDokumen4 halamanHypertonic SolutionsVanessa PaguiriganBelum ada peringkat
- NCP - Acute PainDokumen2 halamanNCP - Acute PainsAm_300% (1)
- NCPDokumen3 halamanNCPeun kyung shinBelum ada peringkat
- Nursing Interventions for Self-Care Deficit and DepressionDokumen3 halamanNursing Interventions for Self-Care Deficit and DepressionDanica Kate GalleonBelum ada peringkat
- NCP For Acute PainDokumen2 halamanNCP For Acute PainEmman RamosBelum ada peringkat
- FNCP Proper SanitationDokumen2 halamanFNCP Proper SanitationgohoonaBelum ada peringkat
- Ate Gara NCP (Activity Intolerance)Dokumen2 halamanAte Gara NCP (Activity Intolerance)Kimsha ConcepcionBelum ada peringkat
- Colorectal Cancer NCP and FDAR FinalDokumen8 halamanColorectal Cancer NCP and FDAR Finalnot your medz duranBelum ada peringkat
- Novilyn C. Pataray BSN - Ii: Assessment Diagnosi S Pathophysiolog Y Planning Interevention Rationale EvaluationDokumen1 halamanNovilyn C. Pataray BSN - Ii: Assessment Diagnosi S Pathophysiolog Y Planning Interevention Rationale EvaluationCharina AubreyBelum ada peringkat
- NCP For Activity IntoleranceDokumen1 halamanNCP For Activity IntoleranceKristine LonyenBelum ada peringkat
- Compromised Family Coping NCPDokumen2 halamanCompromised Family Coping NCPJamaeka Gotis100% (1)
- Now, Try Some Big Leap.: Keep GoingDokumen2 halamanNow, Try Some Big Leap.: Keep GoingShyla ManguiatBelum ada peringkat
- NCP Risk For InfectionDokumen1 halamanNCP Risk For InfectionFielMendozaBelum ada peringkat
- Nursing Care Plan: DATE: 6/27/19Dokumen5 halamanNursing Care Plan: DATE: 6/27/19Maricris Tac-an Calising-PallarBelum ada peringkat
- Assessing and Caring for a Patient with Alzheimer's DiseaseDokumen3 halamanAssessing and Caring for a Patient with Alzheimer's Diseaseria_soriano_2Belum ada peringkat
- L&D Careplan 1 KarenDokumen4 halamanL&D Careplan 1 KarenSimran SandhuBelum ada peringkat
- Nursing Care for Impaired MobilityTITLEPreventing Peripheral Neurovascular Issues TITLERelieving Acute Pain from InflammationDokumen4 halamanNursing Care for Impaired MobilityTITLEPreventing Peripheral Neurovascular Issues TITLERelieving Acute Pain from InflammationDaniel Garraton0% (1)
- Family nursing goal of care on proper food storageDokumen2 halamanFamily nursing goal of care on proper food storagekarl montanoBelum ada peringkat
- Nursing Care PlanDokumen3 halamanNursing Care Planjnx_anonymousBelum ada peringkat
- Nursing Care Plan for Rheumatoid ArthritisDokumen3 halamanNursing Care Plan for Rheumatoid ArthritisJashAnia MarIe EvArdo FloresBelum ada peringkat
- Difficulty Breathing Intervention and EvaluationDokumen1 halamanDifficulty Breathing Intervention and EvaluationJamaica Leslie NovenoBelum ada peringkat
- Nursing Care Plan: Determine Cause of Activity - Determining The Cause of A Disease CanDokumen2 halamanNursing Care Plan: Determine Cause of Activity - Determining The Cause of A Disease Canrix07Belum ada peringkat
- FNCP Risk For InfectionDokumen4 halamanFNCP Risk For InfectionAemz Alacasnap Ainegud0% (1)
- NCP DiarrheaDokumen2 halamanNCP DiarrheaMiguelMartinBelum ada peringkat
- Self Care Deficit BahtingDokumen1 halamanSelf Care Deficit BahtingNaj SoliveresBelum ada peringkat
- Ineffective Health Maintenance Causes and SolutionsDokumen1 halamanIneffective Health Maintenance Causes and Solutionsdragon3466Belum ada peringkat
- Teething:diaper Dermatitis NCPDokumen2 halamanTeething:diaper Dermatitis NCPMARK OLVIER E. MELCHORBelum ada peringkat
- NCPDokumen3 halamanNCPChrisTine M. MoralesBelum ada peringkat
- NCP 2 LRDR For PrintDokumen2 halamanNCP 2 LRDR For PrintGeorge PandaBelum ada peringkat
- Infection NCPDokumen1 halamanInfection NCPMsOrangeBelum ada peringkat
- Cue Problem Scientific Explanation Planning Interventions Rationale EvaluationDokumen5 halamanCue Problem Scientific Explanation Planning Interventions Rationale EvaluationJanyn Abella ReyesBelum ada peringkat
- Anemia in Children CBC (Complete Blood Count)Dokumen4 halamanAnemia in Children CBC (Complete Blood Count)Edraline LumawigBelum ada peringkat
- NCP RiskDokumen3 halamanNCP RiskMaricar Azolae MascualBelum ada peringkat
- Deficit)Dokumen2 halamanDeficit)Lee DeeBelum ada peringkat
- Forro Intestinal ObstructionDokumen3 halamanForro Intestinal ObstructionShiehan Mae ForroBelum ada peringkat
- Forro Intestinal Obstruction-2Dokumen4 halamanForro Intestinal Obstruction-2Shiehan Mae ForroBelum ada peringkat
- Diagnostic Findings:: Short Term Goal Short Term GoalDokumen3 halamanDiagnostic Findings:: Short Term Goal Short Term GoalGiselle EstoquiaBelum ada peringkat
- Name: Grace AGE: 28 Gender: Female Assessment Nursing Diagnosis Objectives Nursing Intervention Rationale Evaluation Subjective: GeneralDokumen2 halamanName: Grace AGE: 28 Gender: Female Assessment Nursing Diagnosis Objectives Nursing Intervention Rationale Evaluation Subjective: GeneralRainier IbarretaBelum ada peringkat
- NURSING CARE PLAN FOR APPENDICITISDokumen7 halamanNURSING CARE PLAN FOR APPENDICITISHanz Abbigail Roco100% (1)
- Osteoporosis Prognosis and Nursing CareDokumen4 halamanOsteoporosis Prognosis and Nursing CareJanine Mae MacaraigBelum ada peringkat
- Knowledge DdeficitDokumen2 halamanKnowledge DdeficitnovagaryBelum ada peringkat
- Aiza NCPDokumen6 halamanAiza NCPponponolmedoBelum ada peringkat
- NCP Drug Study KriziaDokumen5 halamanNCP Drug Study KriziaAlexia AlbaniaBelum ada peringkat
- 12 - Chapter 2Dokumen57 halaman12 - Chapter 2Jo Chiko FlorendoBelum ada peringkat
- 04chapter4pp164 236 PDFDokumen73 halaman04chapter4pp164 236 PDFJo Chiko FlorendoBelum ada peringkat
- Physical Activity For Mood JournalDokumen25 halamanPhysical Activity For Mood JournalJo Chiko FlorendoBelum ada peringkat
- Thesis Format CLDDokumen5 halamanThesis Format CLDJo Chiko FlorendoBelum ada peringkat
- Medical Certificate PDFDokumen3 halamanMedical Certificate PDFarpitha kBelum ada peringkat
- The Level of Physical Activity of University StudeDokumen4 halamanThe Level of Physical Activity of University StudeJo Chiko FlorendoBelum ada peringkat
- GPAQ Analysis GuideDokumen23 halamanGPAQ Analysis GuideThe-Queen Wicked-YglesiasBelum ada peringkat
- Phil Health ProposalDokumen1 halamanPhil Health ProposalJo Chiko FlorendoBelum ada peringkat
- Promissory Note FormsDokumen4 halamanPromissory Note FormsmarkBelum ada peringkat
- Drug StudyDokumen4 halamanDrug StudyJo Chiko FlorendoBelum ada peringkat
- San Lazaro Hospital: Pulmonary TuberculosisDokumen3 halamanSan Lazaro Hospital: Pulmonary TuberculosisJo Chiko FlorendoBelum ada peringkat
- Typhoid FeverDokumen4 halamanTyphoid FeverJo Chiko FlorendoBelum ada peringkat
- Nursing Diagnoses in Psyciatric PDFDokumen734 halamanNursing Diagnoses in Psyciatric PDFEgi MunandarBelum ada peringkat
- Herpes ZosterDokumen2 halamanHerpes ZosterJo Chiko FlorendoBelum ada peringkat
- DESCO Candidate Application InformationDokumen1 halamanDESCO Candidate Application InformationShaat Ronger RongdhonuBelum ada peringkat
- Harold A. Abella - CBC - Ed 5 and Ed 6 - ReviewerDokumen6 halamanHarold A. Abella - CBC - Ed 5 and Ed 6 - ReviewerABELLA, HAROLD A.Belum ada peringkat
- Mental Status Examination: Table 1-6Dokumen8 halamanMental Status Examination: Table 1-6Đức Nguyên VũBelum ada peringkat
- Master Teachers: Implementing Rules and RegulationsDokumen19 halamanMaster Teachers: Implementing Rules and RegulationsChristine PobleteBelum ada peringkat
- Certified Energy Auditor™ Instructions & Application HandbookDokumen26 halamanCertified Energy Auditor™ Instructions & Application Handbookssk3712Belum ada peringkat
- Difficulties On Using English Language Within Grade 12-HumssDokumen5 halamanDifficulties On Using English Language Within Grade 12-HumssMa Alith Frisha BaybayBelum ada peringkat
- 1495082308ePGEDN 10.5 EtextDokumen11 halaman1495082308ePGEDN 10.5 EtextKanchanBelum ada peringkat
- Silfia Dwi AndriatiDokumen111 halamanSilfia Dwi AndriatiWahyuni SusantiBelum ada peringkat
- TWI EssentialsDokumen1 halamanTWI Essentialssjaak0% (1)
- NCR Rncres No1 s2013Dokumen2 halamanNCR Rncres No1 s2013Anjie NovenoBelum ada peringkat
- Interactive Reading ModelDokumen27 halamanInteractive Reading ModelLau Kai Ying0% (1)
- Fall 2021 Master Course MemoDokumen205 halamanFall 2021 Master Course MemoIbrahim MoazzamBelum ada peringkat
- Schools of LinguisticsDokumen3 halamanSchools of LinguisticsWalid WacBelum ada peringkat
- Activate Your Child's Hidden Potential with Mid Brain ActivationDokumen22 halamanActivate Your Child's Hidden Potential with Mid Brain ActivationDhanashri OzaBelum ada peringkat
- Story stem narratives in clinical researchDokumen8 halamanStory stem narratives in clinical researchCristina TatomirBelum ada peringkat
- Mathsphere: MathematicsDokumen6 halamanMathsphere: MathematicsVangapanduSrinivasaraoBelum ada peringkat
- Vineet Kumar CV: Corporate LawyerDokumen4 halamanVineet Kumar CV: Corporate LawyerSaurabh KumarBelum ada peringkat
- Scheme Guidelines for Industry Institute Partnership CellDokumen28 halamanScheme Guidelines for Industry Institute Partnership CellhariselvarajBelum ada peringkat
- Scat3: Sport Concussion Assessment Tool - 3rd EditionDokumen4 halamanScat3: Sport Concussion Assessment Tool - 3rd EditionPhil ThomsonBelum ada peringkat
- RSCH 2122 WEEK 1-10: Learning Activity 1Dokumen14 halamanRSCH 2122 WEEK 1-10: Learning Activity 1Murline UddinBelum ada peringkat
- Alyssa Ortiz Stem ResumeDokumen2 halamanAlyssa Ortiz Stem Resumeapi-645649902Belum ada peringkat
- IELTS General Training Practice Test PDFDokumen58 halamanIELTS General Training Practice Test PDFEmmanuel Tunde Olugbile67% (3)
- Employee Attrition and Retention ChallengesDokumen16 halamanEmployee Attrition and Retention ChallengesJatin GeraBelum ada peringkat
- Language Communities and Societies ExplainedDokumen3 halamanLanguage Communities and Societies ExplainedDhyBelum ada peringkat
- Transfer Learning For Cloud Image ClassificationDokumen4 halamanTransfer Learning For Cloud Image ClassificationStefan WinklerBelum ada peringkat
- Communication Management in Project Management PDFDokumen2 halamanCommunication Management in Project Management PDFMelodyBelum ada peringkat
- How To Write A Winning Grant ProposalDokumen12 halamanHow To Write A Winning Grant Proposalqueztlurv100% (1)
- Mechanical Engineer CV TemplateIE PDFDokumen2 halamanMechanical Engineer CV TemplateIE PDFMadhusudhanan ChelliahBelum ada peringkat
- Ece PDFDokumen157 halamanEce PDFrafi skBelum ada peringkat
- Title of The Program: Fueling Students' Grammatical Skill On Subject-Verb AgreementDokumen6 halamanTitle of The Program: Fueling Students' Grammatical Skill On Subject-Verb AgreementTCHR KIMBelum ada peringkat