UTI
Diunggah oleh
marv43Deskripsi Asli:
Hak Cipta
Format Tersedia
Bagikan dokumen Ini
Apakah menurut Anda dokumen ini bermanfaat?
Apakah konten ini tidak pantas?
Laporkan Dokumen IniHak Cipta:
Format Tersedia
UTI
Diunggah oleh
marv43Hak Cipta:
Format Tersedia
Caused when bacteria get into the urine (rarely viral or fungal) Bacteria usually from the bowel
E.coli causes 80-85%
Staphylococcus saprophyticus causes 10-15% Also Klebsiella, Proteus, Pseudomonas,
Enterobacter
Lower urinary tract is cystitis Upper urinary tract is pyelonephritis
Common bacterial infection in infants and children More frequently in girls, particularly around the age of toilet teaching Other risk factors:
Abnormality in structure or function of urinary tract Abnormal backward flow Vesicoureteral reflux (VUR)
A small percentage (0.33%) with recurrent UTI can develop chronic kidney disease as an adult
seen in 30-50% children with UTI Poor hygiene or toileting habits Use of irritants soap, bubble bath Family history of UTI
Often difficult to recognise due to non-specific symptoms and signs which can include:
In older children symptoms can be similar to those in adults:
Irritability Poor feeding Vomiting Fever
Pain, burning, stinging or urination Urgency and frequency Nocturia Wetting problems, even when toilet taught Abdominal or lower back pain Urine that is foul-smelling, cloudy or contains blood
Definitive diagnosis is not always possible in this age group as it is difficult to obtain a urine sample:
In babies-a plastic bag or absorbent pad to collect the
A positive urine culture is necessary for definitive diagnosis NICE only recommends imaging (ultrasound, DMSA, MCUG) for diagnosis in those less than 6 months, with an atypical UTI or with recurrent UTIs
urine In young children catch in a specimen bottle while they are passing urine If unable to obtain noninvasively, a catheter or suprapubic aspiration may be used (ultrasound first)
Normally hospitalisation is not necessary, but can occur if:
The child has high fever or looks very ill, or there is
a probable kidney infection The child is younger than 6 months old Bacteria from the infected urinary tract may have spread to the blood The child is dehydrated (has low levels of body fluids) or is vomiting and cannot take any fluids or medication by mouth
For infants and children 3 months or older:
Treat with oral antibiotics for 3 days. The choice of
antibiotics should be directed by locally developed multidisciplinary guidance. Trimethoprim, nitrofurantoin, cephalosporin or amoxicillin may be suitable The parents or carers should be advised to bring the infant or child for reassessment if the infant or child is still unwell after 2448 hours
For infants and children 3 months or older:
Consider referral to a paediatric specialist Treat with oral antibiotics for 710 days. The use
of an oral antibiotic with low resistance patterns is recommended, for example cephalosporin or coamoxiclav If oral antibiotics cannot be used, treat with an IV antibiotic such as cefotaxime or ceftriaxone for 2 4 days followed by oral antibiotics for a total duration of 10 days
Most children will recover fine, but some, especially those who are very young when they have their first infection or who have recurrent infections may need further testing to rule out urinary tract abnormalities
Prophylactic antibiotics should only be considered with recurrent UTI Asymptomatic bacteriuria should not be treated prophylactically Dysfunctional elimination syndromes and constipation should be addressed Children who have had a UTI should be encouraged to drink an adequate amount Children who have had a UTI should have ready access to clean toilets when required and should not be expected to delay voiding.
Common infection in children Most are treated with a short course of antibiotics If recurrent need further testing to see in underlying pathology Good hygiene and toilet training can help to prevent Should not cause urinary tract problems as an adult
Anda mungkin juga menyukai
- Shoe Dog: A Memoir by the Creator of NikeDari EverandShoe Dog: A Memoir by the Creator of NikePenilaian: 4.5 dari 5 bintang4.5/5 (537)
- The Yellow House: A Memoir (2019 National Book Award Winner)Dari EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Penilaian: 4 dari 5 bintang4/5 (98)
- Presentation 1Dokumen1 halamanPresentation 1marv43Belum ada peringkat
- Psychiatry MnemonicsDokumen7 halamanPsychiatry MnemonicsFahad Almalki93% (15)
- Presentation 1Dokumen1 halamanPresentation 1marv43Belum ada peringkat
- Asthma: A Talk by Joe and MarvDokumen13 halamanAsthma: A Talk by Joe and Marvmarv43Belum ada peringkat
- Never Split the Difference: Negotiating As If Your Life Depended On ItDari EverandNever Split the Difference: Negotiating As If Your Life Depended On ItPenilaian: 4.5 dari 5 bintang4.5/5 (838)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceDari EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RacePenilaian: 4 dari 5 bintang4/5 (890)
- Grit: The Power of Passion and PerseveranceDari EverandGrit: The Power of Passion and PerseverancePenilaian: 4 dari 5 bintang4/5 (587)
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeDari EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifePenilaian: 4 dari 5 bintang4/5 (5794)
- The Little Book of Hygge: Danish Secrets to Happy LivingDari EverandThe Little Book of Hygge: Danish Secrets to Happy LivingPenilaian: 3.5 dari 5 bintang3.5/5 (399)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureDari EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FuturePenilaian: 4.5 dari 5 bintang4.5/5 (474)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryDari EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryPenilaian: 3.5 dari 5 bintang3.5/5 (231)
- The Emperor of All Maladies: A Biography of CancerDari EverandThe Emperor of All Maladies: A Biography of CancerPenilaian: 4.5 dari 5 bintang4.5/5 (271)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersDari EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersPenilaian: 4.5 dari 5 bintang4.5/5 (344)
- On Fire: The (Burning) Case for a Green New DealDari EverandOn Fire: The (Burning) Case for a Green New DealPenilaian: 4 dari 5 bintang4/5 (73)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaDari EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaPenilaian: 4.5 dari 5 bintang4.5/5 (265)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyDari EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyPenilaian: 3.5 dari 5 bintang3.5/5 (2219)
- Team of Rivals: The Political Genius of Abraham LincolnDari EverandTeam of Rivals: The Political Genius of Abraham LincolnPenilaian: 4.5 dari 5 bintang4.5/5 (234)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreDari EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You ArePenilaian: 4 dari 5 bintang4/5 (1090)
- Rise of ISIS: A Threat We Can't IgnoreDari EverandRise of ISIS: A Threat We Can't IgnorePenilaian: 3.5 dari 5 bintang3.5/5 (137)
- The Unwinding: An Inner History of the New AmericaDari EverandThe Unwinding: An Inner History of the New AmericaPenilaian: 4 dari 5 bintang4/5 (45)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)Dari EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Penilaian: 4.5 dari 5 bintang4.5/5 (119)
- Her Body and Other Parties: StoriesDari EverandHer Body and Other Parties: StoriesPenilaian: 4 dari 5 bintang4/5 (821)
- Engb546 NP RevisedDokumen5 halamanEngb546 NP RevisedRafaelaBelum ada peringkat
- Binomial TheoremDokumen57 halamanBinomial Theoremkailasbankar96Belum ada peringkat
- Present Simple Tense ExplainedDokumen12 halamanPresent Simple Tense ExplainedRosa Beatriz Cantero DominguezBelum ada peringkat
- Case DurexDokumen3 halamanCase DurexGia ChuongBelum ada peringkat
- Engineering: Ronnapee Chaichaowarat, Jun Kinugawa, Kazuhiro KosugeDokumen8 halamanEngineering: Ronnapee Chaichaowarat, Jun Kinugawa, Kazuhiro Kosugelaura bemudezBelum ada peringkat
- Listening LP1Dokumen6 halamanListening LP1Zee KimBelum ada peringkat
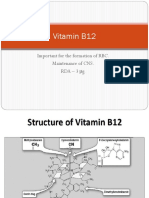
- Vitamin B12: Essential for RBC Formation and CNS MaintenanceDokumen19 halamanVitamin B12: Essential for RBC Formation and CNS MaintenanceHari PrasathBelum ada peringkat
- Problems of Education in The 21st Century, Vol. 78, No. 4, 2020Dokumen199 halamanProblems of Education in The 21st Century, Vol. 78, No. 4, 2020Scientia Socialis, Ltd.Belum ada peringkat
- The Way To Sell: Powered byDokumen25 halamanThe Way To Sell: Powered bysagarsononiBelum ada peringkat
- Assignment Chemical Bonding JH Sir-4163 PDFDokumen70 halamanAssignment Chemical Bonding JH Sir-4163 PDFAkhilesh AgrawalBelum ada peringkat
- So Neither or NorDokumen2 halamanSo Neither or NorMita KusniasariBelum ada peringkat
- Class 7 CitationDokumen9 halamanClass 7 Citationapi-3697538Belum ada peringkat
- Written Arguments of Maintenance Case On Behalf of PetitionerDokumen4 halamanWritten Arguments of Maintenance Case On Behalf of PetitionerSridhara babu. N - ಶ್ರೀಧರ ಬಾಬು. ಎನ್85% (53)
- CV Jan 2015 SDokumen4 halamanCV Jan 2015 Sapi-276142935Belum ada peringkat
- The Space of Reflection: Thirdness and Triadic Relationships in Family TherapyDokumen19 halamanThe Space of Reflection: Thirdness and Triadic Relationships in Family TherapyTasos TravasarosBelum ada peringkat
- Course Outline Physics EducationDokumen3 halamanCourse Outline Physics EducationTrisna HawuBelum ada peringkat
- UTS - Comparative Literature - Indah Savitri - S1 Sastra Inggris - 101201001Dokumen6 halamanUTS - Comparative Literature - Indah Savitri - S1 Sastra Inggris - 101201001indahcantik1904Belum ada peringkat
- Dmat ReportDokumen130 halamanDmat ReportparasarawgiBelum ada peringkat
- Vietnamese Grammar Questions and Answers DocumentDokumen1 halamanVietnamese Grammar Questions and Answers DocumentMinJenBelum ada peringkat
- Cartha Worth SharingDokumen27 halamanCartha Worth SharingtereAC85Belum ada peringkat
- International Journal of Current Advanced Research International Journal of Current Advanced ResearchDokumen4 halamanInternational Journal of Current Advanced Research International Journal of Current Advanced Researchsoumya mahantiBelum ada peringkat
- Movie Recommendation System-1Dokumen25 halamanMovie Recommendation System-1Singi TejaswiniBelum ada peringkat
- Personal Branding dan Positioning Mempengaruhi Perilaku Pemilih di Kabupaten Bone BolangoDokumen17 halamanPersonal Branding dan Positioning Mempengaruhi Perilaku Pemilih di Kabupaten Bone BolangoMuhammad Irfan BasriBelum ada peringkat
- Solutions To Basic Economic Problems - AllDokumen27 halamanSolutions To Basic Economic Problems - AllAsha GeorgeBelum ada peringkat
- Integrating GrammarDokumen8 halamanIntegrating GrammarMaría Perez CastañoBelum ada peringkat
- A Case Study On Implementing ITIL in Bus PDFDokumen7 halamanA Case Study On Implementing ITIL in Bus PDFsayeeBelum ada peringkat
- Khin Thandar Myint EMPADokumen101 halamanKhin Thandar Myint EMPAAshin NandavamsaBelum ada peringkat
- Masala Kitchen Menus: Chowpatty ChatDokumen6 halamanMasala Kitchen Menus: Chowpatty ChatAlex ShparberBelum ada peringkat
- Q2 SHS Intro To World Religion - Module 2Dokumen19 halamanQ2 SHS Intro To World Religion - Module 2jan roiBelum ada peringkat
- (123doc) - Internship-Report-Improving-Marketing-Strategies-At-Telecommunication-Service-Corporation-Company-VinaphoneDokumen35 halaman(123doc) - Internship-Report-Improving-Marketing-Strategies-At-Telecommunication-Service-Corporation-Company-VinaphoneK59 PHAN HA PHUONGBelum ada peringkat