Vol06 b3 14-17p PDF
Diunggah oleh
Ibnu YudistiroJudul Asli
Hak Cipta
Format Tersedia
Bagikan dokumen Ini
Apakah menurut Anda dokumen ini bermanfaat?
Apakah konten ini tidak pantas?
Laporkan Dokumen IniHak Cipta:
Format Tersedia
Vol06 b3 14-17p PDF
Diunggah oleh
Ibnu YudistiroHak Cipta:
Format Tersedia
Journal of IMAB - Annual Proceeding (Scientific Papers) 2006, book 3
ETIOLOGY OF COMMON CONTACT DERMATITIS
S. Racheva Department of Dermatology and Venerology, Medical University Prof. Dr. Paraskev Stoyanov Varna, Bulgaria
RESUME: Contact dermatites (allergic and non-allergic) are frequently observed dermatoss and they pose a serious problem to the dermatologist. They are usually common dermatites, but a considerable number of the cases are occupational dermatites. The clarification of each concrete case is of great significance for a precise therapeutic approach and efficient prophylactics. The study aimed at etiological and pathogenetic clarification of common contact dermatitis in a group of 210 patients. The clarification was achieved through dynamic clinical study, anamnestic data, and skin tests (epicutaneous tests chamber method). In 123 patients (58.5%) of all studied patients allergic contact dermatitis was diagnosed, and in 87 patients (41.4%) irritant contact dermatitis. The analysis of the received 213 positive epicutaneous tests revealed that detergents are the most frequent allergens (16.43%), followed by metals (15.02%), rubber additives (14.80%), parabens (10.79%), antiseptics (10,32%), formaldehyde (9.38%), and scents (8.92%). The most frequent irritant etiological agents were detergents (28.73%), followed by soaps (27.58%), additives to rubber (13.79%), acids and bases, organic solvents. Key words: allergic contact dermatitis, irritant contact dermatitis, contact allergens, contact irritants. The common contact dermatitis cause serious problems in a dermatologists practice. They occur frequently; they are etiopathogenetically different from the allergic contact dermatitis (ACD) with a frequency of 54% (19), and the irritant contact dermatitis (ICD) with a frequency of 27%(19). The most frequent allergens, causing ACD are: nickel and other metals (7,16,20), rubber additives (16,19,20), scents (16,20), formaldehyde (19), preservatives (7), detergents (4), airborne allergens (14). The most frequent irritants, causing ICD are: soaps, detergents, alcohol and other solutions, latex particles (18), strong acids and bases, organic and non-organic salts (9). ACD has undoubtedly allergic genesis (delayed allergic reaction), and ICD is assumed to be a non-immunologic skin irritation. The clinical occurrences, as well as the histological pictures of ACD and ICD are actually different.
In ACD histologically are presented vesiculous formations, inflammatory infiltrate and spongiosa, whereas in ICD - destruction of the corneal layers, intraepidermal necrosis (5). The diagnostics of ACD and ICD is based on many criteria: clinical occurrences, anamnestic data of a connection of the exacerbation with concrete external noxa, clinical observation of the dynamics and laboratory tests. The test methods accentuate on epicutaneous testing with a standard line and additional lines of allergens (1). Several authors recommend histological differentiation between ACD and ICD (5). There are also newer non-invasive in vivo methods for diagnostics of CD (3). There exists a complex interrelation between ACD and ICD the irritant dermatitis or the mere skin irritation predisposes with long exposure to allergization (9) or the eventual transformation of the dermatitis from a common type into an occupational one. This requires that the initial diagnostics for each separate case should be precise and etiologically determined, and that - besides the treatment - an individual prophylactic plan should be developed. The aim of the present paper was the research of the etiology and pathogenesis of the common CD on the grounds of a study of a group of patients in the Clinic of Skin and Venereal Diseases Varna. MATERIALS AND METHODS: The present study includes 210 patients, observed and studied for a period of five years: 123 patients with ACD and 87 patients with ICD. The study was carried out using the method of the covered epicutaneous tests (chamber method), as substances included in the standard line were used as well as other substances selected according to the concrete circumstances. With each patient epicutaneous testing was carried out with 20 standard allergens, and with some patients with some additionally selected allergens. The epicutaneous tests were checked at the 48th hour of their application. The conclusions for the etiological significance of the allergological tests were drawn on grounds of their comparison with anamnestic and clinical data. The differentiation of ACD and ICD was based on the following criteria: clinical picture, anamnestic data, skin tests results, dynamic observation of the cases.
14
RESULTS AND DISCUSSION: Of all the studied patients with CD in 205 patients the etiological cause was proven, as the following distribution in connection with the clinical and pathogenet-
ic diagnosis was established (Table. 1): ACD was established in 123 patients (58.5%) of all the studied, ICD in 87 patients (41.4%), out of whom in 82 patients the etiological cause was established and in 5 patients it remained unclear.
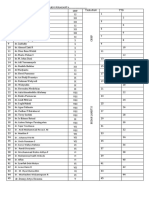
Table 1. Distribution of the patients with contact dermatitis according to clinical and pathogenetic diagnosis (n= 210) Total number of patients 123 Number of patients with positive epicutaneous tests 123
Diagnosis Allergic Contact dermatitis Irritant Contact dermatitis Total
% 58.5
% 100
87 210
41.4 100 123
The analysis of the received 123 positive skin tests in patients with ACD justifies the following conclusions about their etiology (Table.2). Of greatest etiological significance for ACD are: detergents (16.43%), metals (15.02%), rubber additives (14.80%). The groups of
allergenic parabens (10.79%), antiseptics (10.32%), formaldehyde (9.38%) and scents (8.92%) showed considerable frequency as causative agents of ACD. Of smaller frequency turned out to be the Peruvian balsam (7.04%), medicaments (5.16%) and other allergens (2.80%).
Table 2. Etiology of the common allergic contact dermatitis (123 positive epicutaneous tests) Allergens Metals nickel, chromium, cobalt Rubber additives - Thiuram Mix, Phenylendiamin, Diphenyl-p-phenylendiamin, Mercaptobenzthiazol Medicaments neomycin, benzocain, chlornitromycin Formaldehyde Peruvian balsam Scents (Parfum Mix)- cinnamat alcohol, cinnamat aldehyd,Euginol, Isoeuginol, Garanil Parabens (Paraben Mix)- Nipabutyl, Nipagin A, Nipagin M, Nipazol M Detergents Antiseptics Other allergens Total The distribution of the irritant etiological causative agents in the patients with ICD was the following ( Table 3): the most frequent agents are the detergents (28.73%), soaps (27.58%), rubber additives (13.79%), followed by Positive epicutaneous tests 32 % 15.02
30 11 20 15 19 23 35 22 6 213
14.80 5.16 9.38 7.04 8.92 10.79 16,43 10.32 2.8 100
strong bases and acids (10.34% and 8.04%), organic solvents (3.44%) and alcohol solutions (2.29%). In 5 of the studied patients (5.74%) the respective irritant agent remained unclear.
15
Table 3. Etiology of the common irritant contact dermatitis in 87 patients Number of patients with established irritant agent 24 7 9 3 2 25 12 5 87
Irritants Soaps Strong acids Strong bases Organic solvents Alcohol solutions Detergents Rubber Additives Patients with unclear etiological cause Total The received results for contact sensibilization to metals, and above all to nickel, correlate with the data in medical literature. The nickel allergy - globally viewed - is very frequent (16), ranging between 11% and 20% (1,18); it is often occupational and has been decreasing in the last few years (20). Contact with nickel is usually established when trinkets are worn or when metal processing is done professionally. Chromates cause ACD in 6.6% of the cases (1), as they are more often than not professional noxa, and the cobalt chloride in 5.6% (1). Rubber additives also frequently cause ACD (16,19), approximately in 14% of all cases (18). The results of this study are analogical. Of the rubber additives of considerable etiological importance are the latex particles (17), together with the risk agents in this relation atopy, spina bifida etc. (17) and p-phenylendiamin (PPD); the latter having a frequency of 4.1% (1).Contact with this allergen in everyday life and in many professions is very frequent. There are reports of ACD from rubber products (11), from iso-dyes containing PPD and used in the textile and shoe industry. A number of natural dyes used in tattoos contain PPD and cause ACD (12), as does the printer toner. Widely discussed is the cross allergic reaction between PPD and hair dye (8,15) in everyday and professional aspect, as well as the possibility of photoallergic reactions (13). PPD causes a cross allergic reaction also with local anesthetics (10) and with sulphonamides and anti-diabetic medicaments with a similar structure. (15). The etiological significance of the medicaments is a bit more limited: local antibiotics (2), local anesthetics (10),
% 2758 8.04 10.34 3.44 2.29 28.73 13.79 5.74 100
local corticosteroids. Skin occlusion in such cases is discussed as a predisposing factor for the exacerbation of the ACD. The scents also occupy a major place in the etiology of the ACD (16,20), as their frequency ranges between 6.8% (1) and 10% (6). The same holds true of the parabens (7) and the formaldehyde (1,19). The possibility of co-reaction between formaldehyde and glutaraldehid should not be ignored. The Peruvian balsam presents 5% of the ACD cases (6). In everyday life ACD is most often caused by detergents (4), as well as by antiseptics (18). The role of the irritants in the etiology of the CD is significant: 27% according to the data in medical literature (19), 41.4% according to the present study. The most frequent irritants whose effect is felt after a systematic, manifold contact are soaps, detergents, latex particles (18) as well as strong acids, bases, and organic salts whose effect is felt after a single contact (9). CONCLUSIONS: In the etiology of the common ACD of definite importance are the detergents, metals, rubber additives, parabens, antiseptics, formaldehyde and scents, whereas with ICD soaps, other detergents and latex particles. The clarification of the etiology and pathogenesis of the CD is of crucial importance for the accurate therapeutic approach, as well as for justified and efficient prophylactics for each concrete case.
REFERENCES:
1. , . ., . . , . . , , . ., 2001, 1, 17- 21. 2. Assier-Bonnet, H., J. Revuz, Topical neomycin: risk and benefits. Plea for withdrawal, Ann. Deratol Venereol., 1997, 124, 10, 721-5. 3. Aster, S., E. Gonzalez, A. Cheung, F. Rins-Diaz, A. Dukas , F. William , S. Gonzalez Non-Invasive Evaluation of the Kinetics of Allergic and Irritant Contact Dermatits, J. Invest Dermatol., 2005, 124, 351-359.
16
4. Belsito, D., A. F. Fransway, J. F. Fowler et al., Allergic contact dermatitis to detergents: A multicenter study to assess prevalence, J Am.Acad Dermatol, 2002, 46, 200. 5. Brasch, J., J. Burgard, W. Sterry , Common pathogenetic pathways in allergic and irritant contact dermatitis, J. Invest Dermatol, 1992, 98, 166-170. 6. Brown, T., Strategies for prevention: occupational contact dermatitis, Occup Med (Lond.), 2004,54, 7, 450-7. 7. Cohen, D.E., Contact dermatitis: A quarter sentury perspective, J. Am. Acad. Dermatol., 2004,51,60-63. 8. Code-Salazar, L., M. Baz, D. Guimaraens et al., Contact dermatitis in hairdressers: Patch test results in 139 hairdressers (1980-1993), Am J Contact Dermatitis, 1995, 6, 19-23. 9. English, J. S., Current conceps of irritant contact dermatitis, Occup.Environ. Med., 2004 , 61, 722-6, 674.
10. Fischer, A. A., A. Pelzic, N. B. Kanof, The persistence of allergic eczematous sensitivity and the cross-sensitivity pattern to paraphenylendiamine, J. Invest. Dermatol., 30, 1958, 9-12. 11. Fischer, A.A., Nonoccupational dermatitis due black paraphenylendiamine rubber chemicals: Part 1, Cutis, 49, 1992, 163-164. 12. Gallo, R., G. Ghigliotti, E. Gozzani et al., Contact dermatitis from para-phenylendiamine used as a skin paint: A further case, Contact Dermatitis, 1990, 40, 57. 13. Horio, T., Allergic and photoallergic dermatitis from diphenyhydramin, Arch. Dermatol., 112, 1976, 1124-1126. 14. Huygens, S., A. Goossens, An update on airborne contact dermatitis, Contact Dermatitis, 2001, 44, 1, 1-6. 15. Klein, A. D., O. G. Rodman, Allergic contact dermatitis to paraphenylendiamine in hair dye: Case report, Military
Medicine, 1981, 146, 46-47. 16. Kutting, B., R. Brehler, H. Traupe, Allergic contact dermatitis in children: strategies of prevention and risk management, Eur. J. Dermatol., 2004, 14, 2, 805. 17. Michael, T., B. Niggemann, A. Moers et al., Risk factors for latex allergy in patients with spina bifida, Clin. Exp. Allergy, 1996, 26, 934. 18. Nettis, E., M.C. Colanardi, A.L. Soccio, A. Ferrannini, A. Tursi, Occupational irritant and allergic contact dermatitis among healthcare workers, Contact Dermatitis, 2002, 46, 101 107. 19. Templet, J. T., S. Hall, D. V. Belsito, Etiology of hand dermatitis among patients referred for patch testing, Dermatitis, 2004, 15, 1, 25 32. 20. Wesley, N. O., H. I. Maibach, Decreasing allergic contact dermatitis frequency through dermatotoxicologic and epidemiologic based intervention, Food Chem. Toxicol., 2003, 41, 6, 857 60.
Journal of IMAB - Annual Proceeding (Scientific Papers) 2006, book 3
OUR TRAIL IN TREATMENT AND PROPHYLAXIS OF COLD URTICARIA WITH DESLORATADINE
S. Racheva, P. Drumeva, F. Georgieva* Department of Dermatology and Venerology, Medical University Prof. Dr. Paraskev Stoyanov Varna, Bulgaria Medical University and St.Anna Hospital- Varna,
RESUME Cold urticaria presents in quite a lot of cases (31%) with physical urticaria. Its effective treatment and prophylaxis are a problem that is solved by using H1 blockers. Good alternative method nowadays is Desloratadine - Aerius, having maximal effect with minimal risk of adverse reactions. Our study included 30 patients with different forms of cold urticaria: hereditary cold urticaria 4 patients, acquired cold urticaria (contact and refectory) 13 patients, symptomatic cold urticaria (coexisting with viral infections, medicaments, mycoses) - 8 patients, cold cholinergic urticaria 5 patients. All the patients were treated with Desloratadine 1 tablet daily till the end of the clinical features. Afterwards all the patients were prophylacted in the following two months with the same medicament. The results were: the clinical features disappeared in
all the patients in the next 2 weeks; the prophylaxis with Desloratadine was effective in 80% of the treated patients. These allow us to make the conclusion that Desloratadine is a good choice in the treatment and prophylaxis of cold urticaria. INTRODUCTION Cold urticaria presents in quite a lot of cases (31%) with physical urticaria. It can be with acute duration (some weeks) or with long duration (years).There are described cases of cold urticaria associated with vasculitis (5), viral infections (2), and in 2-3% with cryoglobulinemia (15, 18). In most cases it is acquired, determined by IgE (18). Its effective treatment and prophylaxis are a problem that is solved usually by using H1 blockers. They are an effective choice in the treatment of cold urticaria (20, 10, 25).Good results are mentioned by using cyproheptadine as monotherapy (22, 18, 24, 19, 26) or in combination with chlorpheniramin (23)
17
Anda mungkin juga menyukai
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeDari EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifePenilaian: 4 dari 5 bintang4/5 (5794)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreDari EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You ArePenilaian: 4 dari 5 bintang4/5 (1090)
- Never Split the Difference: Negotiating As If Your Life Depended On ItDari EverandNever Split the Difference: Negotiating As If Your Life Depended On ItPenilaian: 4.5 dari 5 bintang4.5/5 (838)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceDari EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RacePenilaian: 4 dari 5 bintang4/5 (895)
- Grit: The Power of Passion and PerseveranceDari EverandGrit: The Power of Passion and PerseverancePenilaian: 4 dari 5 bintang4/5 (588)
- Shoe Dog: A Memoir by the Creator of NikeDari EverandShoe Dog: A Memoir by the Creator of NikePenilaian: 4.5 dari 5 bintang4.5/5 (537)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersDari EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersPenilaian: 4.5 dari 5 bintang4.5/5 (344)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureDari EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FuturePenilaian: 4.5 dari 5 bintang4.5/5 (474)
- Her Body and Other Parties: StoriesDari EverandHer Body and Other Parties: StoriesPenilaian: 4 dari 5 bintang4/5 (821)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)Dari EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Penilaian: 4.5 dari 5 bintang4.5/5 (121)
- The Emperor of All Maladies: A Biography of CancerDari EverandThe Emperor of All Maladies: A Biography of CancerPenilaian: 4.5 dari 5 bintang4.5/5 (271)
- The Little Book of Hygge: Danish Secrets to Happy LivingDari EverandThe Little Book of Hygge: Danish Secrets to Happy LivingPenilaian: 3.5 dari 5 bintang3.5/5 (400)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyDari EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyPenilaian: 3.5 dari 5 bintang3.5/5 (2259)
- The Yellow House: A Memoir (2019 National Book Award Winner)Dari EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Penilaian: 4 dari 5 bintang4/5 (98)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaDari EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaPenilaian: 4.5 dari 5 bintang4.5/5 (266)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryDari EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryPenilaian: 3.5 dari 5 bintang3.5/5 (231)
- Team of Rivals: The Political Genius of Abraham LincolnDari EverandTeam of Rivals: The Political Genius of Abraham LincolnPenilaian: 4.5 dari 5 bintang4.5/5 (234)
- On Fire: The (Burning) Case for a Green New DealDari EverandOn Fire: The (Burning) Case for a Green New DealPenilaian: 4 dari 5 bintang4/5 (73)
- The Unwinding: An Inner History of the New AmericaDari EverandThe Unwinding: An Inner History of the New AmericaPenilaian: 4 dari 5 bintang4/5 (45)
- Allergen Awareness Training PresentationDokumen32 halamanAllergen Awareness Training Presentationaprilia tunggal dewi100% (2)
- Rise of ISIS: A Threat We Can't IgnoreDari EverandRise of ISIS: A Threat We Can't IgnorePenilaian: 3.5 dari 5 bintang3.5/5 (137)
- Drug Allergy BookDokumen332 halamanDrug Allergy Bookmegah_asia13Belum ada peringkat
- VN Shegal Textbook of Clinical Dermatology 5th Edition PDFDokumen365 halamanVN Shegal Textbook of Clinical Dermatology 5th Edition PDFdianaurs1823100% (2)
- Diefenbeck Et Al-2013-International Wound JournalDokumen5 halamanDiefenbeck Et Al-2013-International Wound JournalIbnu YudistiroBelum ada peringkat
- Anterolateral ApproachDokumen3 halamanAnterolateral ApproachHanifBelum ada peringkat
- ABSEN CC NewDokumen3 halamanABSEN CC NewIbnu YudistiroBelum ada peringkat
- Logbook Agustus 2018Dokumen4 halamanLogbook Agustus 2018Ibnu YudistiroBelum ada peringkat
- Quickdash Scoring System: The Quickdash Outcome Measure: Scoring E-Tool For Use by CliniciansDokumen1 halamanQuickdash Scoring System: The Quickdash Outcome Measure: Scoring E-Tool For Use by CliniciansOvidiu RusuBelum ada peringkat
- Quick DashDokumen1 halamanQuick DashIbnu YudistiroBelum ada peringkat
- Quick DashDokumen1 halamanQuick DashIbnu YudistiroBelum ada peringkat
- Quick DashDokumen1 halamanQuick DashIbnu YudistiroBelum ada peringkat
- List RikDokumen20 halamanList RikIbnu YudistiroBelum ada peringkat
- Hypertensive Emergency: Indonesian Society of HypertensionDokumen29 halamanHypertensive Emergency: Indonesian Society of HypertensionRizky Saraswati IndraputriBelum ada peringkat
- Chapter Contents: 8. Maternal ResuscitationDokumen10 halamanChapter Contents: 8. Maternal ResuscitationChristine Notoningtiyas SantosoBelum ada peringkat
- Chapter Contents: 8. Maternal ResuscitationDokumen10 halamanChapter Contents: 8. Maternal ResuscitationChristine Notoningtiyas SantosoBelum ada peringkat
- Mustard Allergy: The FactsDokumen5 halamanMustard Allergy: The FactsAnonymous GBge2ED1OBelum ada peringkat
- Virlix DrugDokumen2 halamanVirlix DrugMsOrangeBelum ada peringkat
- Steven Johnson DiseaseDokumen7 halamanSteven Johnson DiseaseKatrina PonceBelum ada peringkat
- Hypothermia Protocol by WademDokumen53 halamanHypothermia Protocol by WademJE AsuncionBelum ada peringkat
- Anaphylaxis ReactionDokumen27 halamanAnaphylaxis Reactionmau tauBelum ada peringkat
- Skin AsthmaDokumen7 halamanSkin AsthmaJames Domini Lopez LabianoBelum ada peringkat
- Edema of The Uvula: Etiology, Risk Factors, Diagnosis, and TreatmentDokumen4 halamanEdema of The Uvula: Etiology, Risk Factors, Diagnosis, and TreatmentAfri AdiBelum ada peringkat
- UrticariaDokumen9 halamanUrticariaIndah KaDeBelum ada peringkat
- Drug Allergy by Alison ThorpeDokumen13 halamanDrug Allergy by Alison ThorpeAlison ThorpeBelum ada peringkat
- WAO White Book On Allergy PDFDokumen238 halamanWAO White Book On Allergy PDFAura Lorena Rivas ZambranoBelum ada peringkat
- Autacoids: Definition: Chemical Substances Produced LocallyDokumen23 halamanAutacoids: Definition: Chemical Substances Produced LocallyAlphahin 17Belum ada peringkat
- Metrogyl: New Zealand Consumer Medicine InformationDokumen4 halamanMetrogyl: New Zealand Consumer Medicine InformationAnbu KrishnanBelum ada peringkat
- Derma CD McqsDokumen22 halamanDerma CD McqsheshamBelum ada peringkat
- RLE 118 REVISED Case Scenario No. 10 Anaphylactic ShockDokumen2 halamanRLE 118 REVISED Case Scenario No. 10 Anaphylactic ShockKiara Denise TamayoBelum ada peringkat
- CV IamandescuDokumen4 halamanCV Iamandescujuanitos111Belum ada peringkat
- AllergyDokumen23 halamanAllergyAmbl GeronBelum ada peringkat
- Allergy - 2021 - Zuberbier - The International EAACI GA LEN EuroGuiDerm APAAACI Guideline For The DefinitionDokumen33 halamanAllergy - 2021 - Zuberbier - The International EAACI GA LEN EuroGuiDerm APAAACI Guideline For The DefinitionAdelina PopescuBelum ada peringkat
- wk8 Nursing Care of A Family When A Child Has An Immune Disorders Part 2Dokumen32 halamanwk8 Nursing Care of A Family When A Child Has An Immune Disorders Part 2claire yowsBelum ada peringkat
- TTM As5000brochureDokumen12 halamanTTM As5000brochureAphichetBelum ada peringkat
- Small Animal DermatologyDokumen278 halamanSmall Animal DermatologyManuel Rodriguez100% (1)
- Acute Angioedema Overview of Angioedema TreatmentDokumen5 halamanAcute Angioedema Overview of Angioedema TreatmentGiorgiana pBelum ada peringkat
- Contact Dermatitis 2015parameterDokumen39 halamanContact Dermatitis 2015parameterSaniya Ilma ArifaBelum ada peringkat
- Chronic UrticariaDokumen4 halamanChronic UrticariaayukBelum ada peringkat
- SI No Indicator Definition Formula Remarks: Percentage of Medication ErrorsDokumen10 halamanSI No Indicator Definition Formula Remarks: Percentage of Medication ErrorskhushbujoshiBelum ada peringkat
- Act. Health 4TH Q.Dokumen1 halamanAct. Health 4TH Q.xiozas cansanayBelum ada peringkat
- Low Histamine Diet Meal Plan PDFDokumen15 halamanLow Histamine Diet Meal Plan PDFEliška KrálikováBelum ada peringkat
- URTICARIADokumen2 halamanURTICARIAChandra Kefi AmtiranBelum ada peringkat