NIH Public Access: Management of Rodent Exposure and Allergy in The Pediatric Population
Diunggah oleh
Resti Zulvanita DeviJudul Asli
Hak Cipta
Format Tersedia
Bagikan dokumen Ini
Apakah menurut Anda dokumen ini bermanfaat?
Apakah konten ini tidak pantas?
Laporkan Dokumen IniHak Cipta:
Format Tersedia
NIH Public Access: Management of Rodent Exposure and Allergy in The Pediatric Population
Diunggah oleh
Resti Zulvanita DeviHak Cipta:
Format Tersedia
NIH Public Access
Author Manuscript
Curr Allergy Asthma Rep. Author manuscript; available in PMC 2014 December 01.
NIH-PA Author Manuscript
Published in final edited form as:
Curr Allergy Asthma Rep. 2013 December ; 13(6): . doi:10.1007/s11882-013-0378-4.
Management of Rodent Exposure and Allergy in the Pediatric
Population
Elizabeth C. Matsui, MD, MHS
Abstract
NIH-PA Author Manuscript
Although rodent allergy has long been recognized as an occupational disease, it has only been in
the past decade that it has been recognized as a community-based disease that affects children.
Most homes in the US have detectable mouse allergen, but the concentrations in inner-city homes
are orders of magnitude higher than those found in suburban homes. Home mouse allergen
exposure has been linked to sensitization to mouse, and children with asthma who are both
sensitized and exposed to high mouse allergen concentrations at home are at greater risk for
symptoms, exacerbations and reduced lung function. Rat allergen is found primarily in inner-city
homes and has also been linked to asthma morbidity among sensitized children. The objective of
this review is to summarize the scientific literature on rodents and their allergens, the effects of
exposure to these allergens on allergic respiratory disease, and to make recommendations, based
on this evidence base, for the evaluation and management of mouse allergy in the pediatric
population.
Keywords
Childhood asthma; Inner-city asthma; Rodent allergens; Environmental intervention; Integrated
pest management; Pediatric; Rodent exposure; Allergy; Sensitization
Introduction
NIH-PA Author Manuscript
The major mouse allergen, Mus m 1, is a 1619kD lipocalin that is excreted in large
amounts in the urine, but can also be found in other biologic material such as epithelium.(1,
2) Mus m 1 is a pheromone binding protein that is involved in mating habits and its
production is regulated by sex steroids so that it is found in much higher quantities in urine
from male than female mice.(3) It is carried on small particles, with the bulk of it found on
particles 10 microns or less in diameter,(4) so that it is readily airborne and remains so for
prolonged periods of time. In occupational settings, it is detected in air samples collected
from areas away from mice and is thought to travel from one location to another by a
combination of airborne travel and transfer of the allergen on peoples clothing.(46) A
second mouse allergen, Mus m 2, has also been described and is found primarily in hair and
dander(1). Rat n 1 is the major rat allergen and has high homology with Mus m 1.(7) It, too,
is a pheromone binding protein of the lipocalin family that is primary excreted in urine. It is
also carried on small particles so is readily detectable in the air.
Corresponding author: Elizabeth C. Matsui, MD, MHS, The Johns Hopkins Hospital, CMSC 1102, 600 N. Wolfe Street, Baltimore,
MD 21287, T: 410.502.3858, F: 410.955.0229, ematsui@jhmi.edu.
Human and Animal Rights and Informed Consent
This article does not contain any studies with human or animal subjects performed by any of the authors.
Conflict of Interest
Elizabeth C. Matsui has served on an EPA Science Advisory Board, received honoraria from ThermoFisher, and received durable
goods support for asthma studies from 3M and Clean Brands LLC.
Matsui
Page 2
Exposure in Community Settings
NIH-PA Author Manuscript
NIH-PA Author Manuscript
Mus m 1 is found in settled dust samples from almost all inner-city homes(8) and 7580%
of US homes.(912) Although the prevalence of the allergen is high even in suburban
communities, the concentration of mouse allergen varies greatly between inner-city
communities and non-inner-city communities, with concentrations being as much as 1000fold greater in inner-cities. In one study of inner-city children with asthma, >85% of
bedroom air samples had detectable mouse allergen, and approximately 25% had airborne
concentrations similar to those seen in some occupational settings.(10) However, even
among inner-city communities there is variability in mouse allergen concentrations. Innercity neighborhoods in the Northeastern and Midwestern US cities tend to have higher
concentrations than inner-city neighborhoods in the West.(13) In addition, certain home
characteristics have been associated with higher concentrations of mouse allergen and these
include presence of holes or cracks in the walls or doors; report of mouse sightings; and
presence or report of cockroaches.(8, 14, 15) The presence of a cat in the home is associated
with lower mouse allergen concentrations; however, in our studies, most inner-city children
with asthma who are mouse sensitized are also cat sensitized, so acquiring a cat is not a
viable strategy for trying to improve asthma in this population. Although children should not
be exposed directly through occupational sources, one study suggests that adults who work
with rodents may passively transfer allergen from their work environments to their homes.
(16) Children are, however, exposed in schools and daycares, and in some cases may be
exposed to higher levels at school than at home.(17, 18) Rat allergen has been studied less
than mouse allergen; one multi-center inner-city asthma study found that it was detectable in
approximately one-third of settled dust samples from inner-city homes.(19) The difference
in prevalence of rat and mouse allergens is consistent with the behaviors of these two
rodents as rats tend to be outdoor dwellers and mice indoor dwellers.
Sensitization
Children with persistent asthma from urban communities should be evaluated for mouse
sensitization. The currently available tools include allergy skin testing and specific IgE
testing. Commercially available extracts in the US are mouse epithelial extracts, and are not
urinary extracts. The extracts are also not standardized and there is likely at least a ten-fold
range in the Mus m 1 concentration of these extracts.(20) Specific IgE tests are available on
the ImmunoCAP platform for mouse urine, mouse epithelium, and mouse serum, and nasal
challenge studies in adults suggest that mouse urine specific IgE and/or skin prick testing are
the best tests for identifying clinically-relevant sensitization.(20) To my knowledge,
diagnostic testing for rat allergy in community populations has not been studied.
NIH-PA Author Manuscript
The prevalence of mouse sensitization varies from community to community, with one
multi-center study finding that 18% of inner-city asthmatics are sensitized,(21) but in some
inner-city communities as many as 50% are sensitized.(22) Prevalence of sensitization in
suburban and rural asthmatics is approximately 1213%,(11, 23) but the overall prevalence
of mouse-specific IgE in the US population is only 1%(24); however, some of the difference
in sensitization prevalence between these two types of populations may be due to use of skin
testing in the asthmatic populations and specific IgE testing in the US population-based
survey. The prevalence of sensitization to rat in the US population is also 1%,(24) which is
not surprising given the high degree of homology at the amino acid level between mouse
and rat allergens,(25) and our own observation in occupational and inner-city asthma
populations is that sensitization to the two allergens is highly concordant.
Curr Allergy Asthma Rep. Author manuscript; available in PMC 2014 December 01.
Matsui
Page 3
Immunologic and Health Effects of Rodent Allergen Exposure
NIH-PA Author Manuscript
Mouse sensitization is associated with home mouse allergen exposure(21); the risk of
sensitization tends to increase with increasing concentrations of mouse allergen, although
some evidence suggests that the risk of sensitization may be attenuated at extremely high
concentrations of exposure.(26) Mouse-specific IgG is generally associated with exposure
and appears to be common in inner-city children with asthma, but its significance is unclear.
Whether exposure reduction can reduce the risk of developing sensitization remains unclear,
but the lack of success of environmental interventions in primary prevention of sensitization
to other indoor allergens suggests that it is unlikely to be of benefit. In addition, mouse
sensitization in early life is associated with an increased risk of wheeze, rhinitis, and eczema
by age 3 in one inner-city birth cohort, suggesting that it is a risk factor not only for asthma,
but other allergic diseases including rhinitis and eczema.(27)
NIH-PA Author Manuscript
NIH-PA Author Manuscript
Mouse allergen exposure has repeatedly been linked to worse asthma among sensitized
urban children with asthma, particularly in Northeastern and Midwestern US cities.(9, 13,
22) In communities where mouse infestation is common, as many as 40% of children with
persistent, uncontrolled asthma are both sensitized and exposed to mouse allergen,
suggesting that mouse allergen plays an important role in a large proportion of asthmatic
children in these communities. Even though mouse sensitization is uncommon in the US
population as a whole, those who report doctor-diagnosed allergies and are exposed to
higher mouse allergen concentrations have a greater risk of current asthma.(28) Although
several studies have defined exposure as a level above a particular threshold, there appears
to be a dose-response relationship between exposure and asthma morbidity,(29) suggesting
that reductions in home mouse allergen concentrations should result in a reduction in asthma
morbidity. Although mouse allergen concentrations in dust from sites throughout a home are
strongly correlated, mouse allergen concentrations in the bed may be most strongly
associated with a range of clinical markers of asthma, including lung function, exhaled nitric
oxide, and acute visits. Importantly, a recent study of Baltimore children with asthma found
that mouse allergen was the major contributor to asthma morbidity in that community, and
that other major indoor allergens, including cockroach, contributed little to asthma
morbidity.(22) This recent study highlights the fact that mouse allergen may be the major
driver of asthma morbidity in some inner-city communities. With respect to the health
effects of rat allergen in community populations, there are many fewer studies. One multicenter inner-city asthma study reported an association between rat allergen exposure and
asthma morbidity among rat sensitized children.(19) Although rat allergen exposure is likely
an important contributor to asthma morbidity in some children, it is important to note that
only approximately 1/3 of inner-city children with asthma had detectable rat allergen in their
homes, suggesting that fewer children are affected by rat than mouse allergen.
Home Rodent Allergen Interventions
Because of the strong association between home mouse allergen exposure and asthma
morbidity in inner-cities, there is great interest in approaches to reduce home mouse allergen
exposure as a means of improving asthma. One pilot study demonstrated that a
professionally administered integrated pest management intervention reduced mouse
allergen concentrations by at least 75%.(30) This intervention was developed by a pest
management professional and included education regarding best housekeeping practices to
eliminate food sources; emphasis on exclusion work, which includes sealing all holes and
cracks that can serve as entry points for mice; placement of traps; and in heavily infested
homes, application of low toxicity rodenticide out of reach of pets and children.
Recommended housekeeping practices include using food storage containers with lids that
are very difficult for mice to chew through, restricting eating to the kitchen and dining areas
Curr Allergy Asthma Rep. Author manuscript; available in PMC 2014 December 01.
Matsui
Page 4
NIH-PA Author Manuscript
of the home, and sweeping floors and cleaning off countertops immediately after eating.
Since mice can enter homes through holes as small as inch in diameter, careful inspection
with a flashlight and in some cases, an angled mirror, is required to identify potential entry
points. Moving appliances away from walls or surrounding cabinetry is also important for
both cleaning up allergen reservoirs and locating potential entry points. The most commonly
used trap, the snap trap, is very effective and a variety of baits, including peanut butter and
sesame oil, are effective. Bait blocks are not recommended and many pesticides must be
applied by licensed pest management professionals. Similar approaches should be effective
to eradicate rats, but there are scant data in regards to home interventions for rats.
All of the above approaches are useful for removing mice, the source of the allergen, but
additional approaches, in conjunction with integrated pest management, may also help to
reduce allergen concentrations. For example, portable air purifiers are known to reduce
airborne particulate matter by as much as 2550%,(31, 32) and since mouse allergen is
found on these particles, it is possible that air purifiers may be helpful. In addition, the bed is
an important reservoir of mouse allergen and allergen-proof mattress and pillow
encasements that are effective for other animal allergens,(33) which are also found on small
particles, may be a helpful adjunctive strategy for reducing exposure. However, the efficacy
of neither air purifiers nor allergen proof mattress and pillow encasements in reducing
mouse allergen concentrations has been studied.
NIH-PA Author Manuscript
Although it would be reasonable to expect that a substantial reduction of mouse allergen
concentrations would result in an improvement in asthma in sensitized children, this notion
has not been fully tested in a clinical trial. One multi-center randomized controlled trial in
rodent-sensitized asthmatic children was largely negative, but the intervention achieved only
a small reduction in home mouse allergen concentrations (27%), likely because the
intervention was not administered by pest management professionals and primarily relied on
parents/guardians to implement it.(13) Nevertheless, a post-hoc analysis of children whose
homes had at least a 50% reduction in mouse allergen concentrations suggested an
improvement in a couple of quality-of-life related outcomes. A multi-center clinical trial of a
professionally delivered IPM intervention that includes air purifiers and mattress and pillow
encasements is underway and should provide important information about the efficacy of a
comprehensive home intervention aimed at mouse allergen.
Evaluation of Sensitization and Exposure in Pediatric Patients: Practical
Considerations
NIH-PA Author Manuscript
An important consideration in patient evaluation is whether the community in which he/she
resides is likely to have high concentrations of mouse allergen. Assessment of mouse
sensitization is important for children with persistent asthma living in urban areas,
particularly in the Northeastern or Midwestern US. In addition, if the parent reports seeing
evidence of mice (such as droppings, chewed materials) or mice, the patient should also be
assessed for sensitization. Although most of the scientific literature focuses on asthma, at
least one study has linked mouse sensitization to rhinitis,(27) so children with perennial
rhinitis symptoms from urban communities should also be evaluated for mouse sensitization.
As discussed above, either skin prick testing or mouse urine specific IgE testing is
appropriate for evaluation of sensitization (Table 1).
Assessment of exposure is quite feasible in the research setting but difficult in the clinical
setting, particularly when the patients who are affected may not be able to pay out of pocket
for an environmental assessment. In addition to knowledge about mouse infestation in the
community, a history elicited from the parents that they have seen evidence of mice or mice
is very helpful as it provides confirmation that the allergen is present, and potentially present
Curr Allergy Asthma Rep. Author manuscript; available in PMC 2014 December 01.
Matsui
Page 5
NIH-PA Author Manuscript
in high concentrations.(34) A negative history, however, does not rule out clinically relevant
concentrations of mouse allergen, particularly when a patient resides in community where
infestation is common; this patient still deserves assessment of mouse sensitization. A
negative history when a patient resides in a community where infestation is rare suggests
that mouse allergen exposure is very unlikely to be contributing to his/her asthma. It is
important to note, however, that there are home environmental assessment services available
in many communities and that even when this service is not available, a patient can collect a
dust sample from their home and send it to a commercial laboratory for measurement of
mouse allergen. Third party payers do not cover the costs of these services in many cases,
but in some communities these services are available for free through health departments or
non-profit agencies. A high quality licensed professional pest management specialist will
also perform a thorough home assessment as a part of his/her service and be able to provide
an assessment of infestation.
NIH-PA Author Manuscript
If a patient is sensitized and there is reason to suspect exposure in the home, the first step is
to eradicate the source of the allergen, or the mice. There are some steps that families can
take that can be successful in eradicating the infestation;(35) these steps include institution
of housekeeping practices such as those discussed above that eliminate food sources for
mice and identification and sealing of holes through which mice could enter the home.
Using caulk alone has limited effectiveness as mice can chew through the dried caulk.
Instead, use of copper mesh along with caulking material is best. Families should also set
traps and place them in locations where they have seen evidence of mice. In some cases,
pest management services are needed, and a high quality pest management professional
should be employed. Determining which pest management companies provide high quality
service can be challenging, but high quality companies are those that thoroughly inspect the
home (including pulling out appliances in the kitchen, checking for gaps around pipes where
they enter the home, assessing heating units), emphasize exclusion work (sealing of all holes
and cracks), opt for rodenticide only when necessary, and avoid use of bait blocks.
NIH-PA Author Manuscript
In addition to removing the source of the allergen, measures that might help reduce the
concentration of the allergen in the home include washing of all bed linens frequently in hot
water and use of allergen proof mattress and pillow encasements. None of these abatement
measures has been studied for mouse allergen, but they may help reduce exposure to mouse
allergen that has accumulated in bedding. Air purifiers have not been studied for mouse
allergen, but clinical trials indicate that HEPA purifiers reduce airborne particles by at least
2550%, and because mouse allergen is readily airborne, use of air purifiers may reduce
concentrations of mouse allergen in the air. However, given the fact that similar
interventions aimed at reducing pet allergen concentrations when the pet remains in the
home are not very effective, it is likely that the single most important step for reducing home
mouse allergen exposure is eradication of the infestation. Finally, although mouse extracts
for allergen immunotherapy are commercially available, immunotherapy has not been
studied in children with mouse allergy and asthma.
Conclusions
Rodent allergens are a significant cause of asthma morbidity in children, particularly those
living in low-income urban areas. Children with persistent asthma living in communities
where mouse infestation is common, or whose parent reports evidence of mice in the home,
should be assessed for sensitization to mouse. Although eradication of infestation can be
challenging, integrated pest management approaches can result in substantial reductions in
home mouse allergen levels.
Curr Allergy Asthma Rep. Author manuscript; available in PMC 2014 December 01.
Matsui
Page 6
Acknowledgments
NIH-PA Author Manuscript
This work was funded in part by the National Institute of Environmental Health Sciences (P50ES015903,
P01ES018176), the Environmental Protection Agency (R832139), the National Institute of Allergy and Infectious
Diseases (R01AI070630 and U01AI083238), and the Johns Hopkins University School of Medicine General
Clinical Research Center grant number M01-RR00052, from the National Center for Research Resources/NIH.
References
NIH-PA Author Manuscript
NIH-PA Author Manuscript
1. Schumacher MJ. Characterization of allergens from urine and pelts of laboratory mice.
MolImmunol. 1980; 17:10871095.
2. Schumacher MJ, Tait BD, Holmes MC. Allergy to murine antigens in a biological research institute.
JAllergy ClinImmunol. 1981; 68:310318.
3. Sharrow SD, Vaughn JL, Zidek L, Novotny MV, Stone MJ. Pheromone binding by polymorphic
mouse major urinary proteins. Protein Sci. 2002; 11:22472256. [PubMed: 12192080]
4. Ohman JL Jr, Hagberg K, MacDonald MR, Jones RR Jr, Paigen BJ, Kacergis JB. Distribution of
airborne mouse allergen in a major mouse breeding facility. JAllergy ClinImmunol. 1994; 94:810
817.
5. Curtin-Brosnan J, Paigen B, Hagberg KA, Langley S, ONeil EA, Krevans M, Eggleston PA,
Matsui EC. Occupational mouse allergen exposure among non-mouse handlers. J Occup Environ
Hyg. 2010; 7:726734. [PubMed: 21058157]
6. Krop EJ, Doekes G, Stone MJ, Aalberse RC, van der Zee JS. Spreading of occupational allergens:
laboratory animal allergens on hair-covering caps and in mattress dust of laboratory animal workers.
Occup Environ Med. 2007; 64:267272. [PubMed: 17053016]
7. Hilger C, Kuehn A, Hentges F. Animal lipocalin allergens. Curr Allergy Asthma Rep. 2012;
12:438447. [PubMed: 22791068]
8. Phipatanakul W, Eggleston PA, Wright EC, Wood RA. Mouse allergen. I. The prevalence of mouse
allergen in inner-city homes. The National Cooperative Inner-City Asthma Study. JAllergy
ClinImmunol. 2000; 106:10701074.
9. Matsui EC, Eggleston PA, Buckley TJ, Krishnan JA, Breysse PN, Rand CS, Diette GB. Household
mouse allergen exposure and asthma morbidity in inner-city preschool children. AnnAllergy
Asthma Immunol. 2006; 97:514520.
10. Matsui EC, Simons E, Rand C, Butz A, Buckley TJ, Breysse P, Eggleston PA. Airborne mouse
allergen in the homes of inner-city children with asthma. JAllergy ClinImmunol. 2005; 115:358
363.
11. Matsui EC, Wood RA, Rand C, Kanchanaraksa S, Swartz L, Eggleston PA. Mouse allergen
exposure and mouse skin test sensitivity in suburban, middle-class children with asthma. JAllergy
ClinImmunol. 2004; 113:910915.
12. Cohn RD, Arbes SJ Jr, Yin M, Jaramillo R, Zeldin DC. National prevalence and exposure risk for
mouse allergen in US households. JAllergy ClinImmunol. 2004; 113:11671171.
13. Pongracic JA, Visness CM, Gruchalla RS, Evans R 3rd, Mitchell HE. Effect of mouse allergen and
rodent environmental intervention on asthma in inner-city children. Ann Allergy Asthma
Immunol. 2008; 101:3541. [PubMed: 18681082]
14. Chew GL, Perzanowski MS, Miller RL, Correa JC, Hoepner LA, Jusino CM, Becker MG, Kinney
PL. Distribution and determinants of mouse allergen exposure in low-income New York City
apartments. EnvironHealth Perspect. 2003; 111:13481351.
15. Cohn RD, Arbes SJ Jr, Jaramillo R, Reid LH, Zeldin DC. National prevalence and exposure risk
for cockroach allergen in U.S. households. EnvironHealth Perspect. 2006; 114:522526.
16. Krakowiak A, Szulc B, Gorski P. Allergy to laboratory animals in children of parents
occupationally exposed to mice, rats and hamsters. Eur Respir J. 1999; 14:352356. [PubMed:
10515413]
17. Permaul P, Hoffman E, Fu C, Sheehan W, Baxi S, Gaffin J, Lane J, Bailey A, King E, Chapman
M, Gold D, Phipatanakul W. Allergens in urban schools and homes of children with asthma.
Pediatr Allergy Immunol. 2012; 23:543549. This study demonstrated significantly higher
Curr Allergy Asthma Rep. Author manuscript; available in PMC 2014 December 01.
Matsui
Page 7
NIH-PA Author Manuscript
NIH-PA Author Manuscript
NIH-PA Author Manuscript
concentrations of mouse allergen in schools than in homes in one US community. [PubMed:
22672325]
18. Perry TT, Vargas PA, Bufford J, Feild C, Flick M, Simpson PM, Hamilton RG, Jones SM.
Classroom aeroallergen exposure in Arkansas head start centers. Ann Allergy Asthma Immunol.
2008; 100:358363. [PubMed: 18450122]
19. Perry T, Matsui E, Merriman B, Duong T, Eggleston P. The prevalence of rat allergen in inner-city
homes and its relationship to sensitization and asthma morbidity. JAllergy ClinImmunol. 2003;
112:346352.
20. Sharma HP, Wood RA, Bravo AR, Matsui EC. A comparison of skin prick tests, intradermal skin
tests, and specific IgE in the diagnosis of mouse allergy. JAllergy ClinImmunol. 2008; 121:933
939.
21. Phipatanakul W, Eggleston PA, Wright EC, Wood RA. Mouse allergen. II. The relationship of
mouse allergen exposure to mouse sensitization and asthma morbidity in inner-city children with
asthma. JAllergy ClinImmunol. 2000; 106:10751080.
22. Ahluwalia SK, Peng RD, Breysse PN, Diette GB, Curtin-Brosnan J, Aloe C, Matsui EC. Mouse
allergen is the major allergen of public health relevance in Baltimore City. The Journal of allergy
and clinical immunology. 2013 This prospective cohort study found that mouse, but not
cockroach, allergen exposure is the major contributor to asthma morbidity in Baltimore.
23. Welch JE, Hogan MB, Wilson NW. Mouse allergy among asthmatic children from rural
Appalachia. Ann Allergy Asthma Immunol. 2003; 90:223225. [PubMed: 12602670]
24. Gergen PJ, Arbes SJ Jr, Calatroni A, Mitchell HE, Zeldin DC. Total IgE levels and asthma
prevalence in the US population: results from the National Health and Nutrition Examination
Survey 20052006. The Journal of allergy and clinical immunology. 2009; 124:447453.
[PubMed: 19647861]
25. Jeal H, Harris J, Draper A, Taylor AN, Cullinan P, Jones M. Dual sensitization to rat and mouse
urinary allergens reflects cross-reactive molecules rather than atopy. Allergy. 2009; 64:855861.
[PubMed: 19154543]
26. Matsui EC, Eggleston PA, Breysse PN, Rand CS, Diette GB. Mouse allergen-specific antibody
responses in inner-city children with asthma. JAllergy ClinImmunol. 2007; 119:910915.
27. Donohue KM, Al-alem U, Perzanowski MS, Chew GL, Johnson A, Divjan A, Kelvin EA, Hoepner
LA, Perera FP, Miller RL. Anti-cockroach and anti-mouse IgE are associated with early wheeze
and atopy in an inner-city birth cohort. The Journal of allergy and clinical immunology. 2008;
122:914920. [PubMed: 19000580]
28. Salo PM, Jaramillo R, Cohn RD, London SJ, Zeldin DC. Exposure to mouse allergen in U.S.
homes associated with asthma symptoms. Environ Health Perspect. 2009; 117:387391. [PubMed:
19337513]
29. Torjusen EN, Diette GB, Breysse PN, Curtin-Brosnan J, Aloe C, Matsui EC. Dose-response
Relationships between Mouse Allergen Exposure and Asthma Morbidity Among Urban Children
and Adolescents. Indoor Air. 2012 This prospective cohort study found a linear dose-response
relationship between home mouse allergen exposure and asthma morbidity, providing a strong
rationale for home-based environmental interventions targeting mouse allergen.
30. Phipatanakul W, Cronin B, Wood RA, Eggleston PA, Shih MC, Song L, Tachdjian R, Oettgen HC.
Effect of environmental intervention on mouse allergen levels in homes of inner-city Boston
children with asthma. AnnAllergy Asthma Immunol. 2004; 92:420425.
31. Butz AM, Matsui EC, Breysse P, Curtin-Brosnan J, Eggleston P, Diette G, Williams D, Yuan J,
Bernert JT, Rand C. A randomized trial of air cleaners and a health coach to improve indoor air
quality for inner-city children with asthma and secondhand smoke exposure. Arch Pediatr Adolesc
Med. 2011; 165:741748. [PubMed: 21810636]
32. Lanphear BP, Hornung RW, Khoury J, Yolton K, Lierl M, Kalkbrenner A. Effects of HEPA air
cleaners on unscheduled asthma visits and asthma symptoms for children exposed to secondhand
tobacco smoke. Pediatrics. 2011; 127:93101. [PubMed: 21149427]
33. Vaughan JW, McLaughlin TE, Perzanowski MS, Platts-Mills TA. Evaluation of materials used for
bedding encasement: effect of pore size in blocking cat and dust mite allergen. The Journal of
allergy and clinical immunology. 1999; 103:227231. [PubMed: 9949312]
Curr Allergy Asthma Rep. Author manuscript; available in PMC 2014 December 01.
Matsui
Page 8
NIH-PA Author Manuscript
34. Curtin-Brosnan J, Matsui EC, Breysse P, McCormack MC, Hansel NN, Tonorezos ES, Eggleston
PA, Williams DL, Diette GB. Parent report of pests and pets and indoor allergen levels in innercity homes. Ann Allergy Asthma Immunol. 2008; 101:517523. [PubMed: 19055206]
35. Phipatanakul W, Matsui E, Portnoy J, Williams PB, Barnes C, Kennedy K, Bernstein D, BlessingMoore J, Cox L, Khan D, Lang D, Nicklas R, Oppenheimer J, Randolph C, Schuller D, Spector
S, Tilles SA, Wallace D, Sublett J, Bernstein J, Grimes C, Miller JD, Seltzer J. Environmental
assessment and exposure reduction of rodents: a practice parameter. Ann Allergy Asthma
Immunol. 2012; 109:375387. This practice parameter provides a thorough review of
environmental assessment and interventions to reduce mouse allergen exposure. [PubMed:
23176873]
NIH-PA Author Manuscript
NIH-PA Author Manuscript
Curr Allergy Asthma Rep. Author manuscript; available in PMC 2014 December 01.
Matsui
Page 9
TABLE 1
Key points: assessment and management
NIH-PA Author Manuscript
Although mouse allergen is found in most homes in the US, concentrations in urban homes in the Northeastern and Midwestern US
are orders of magnitude higher than other homes in the US.
Skin prick testing and/or specific IgE testing are useful for identifying patients with clinically relevant sensitization.
Although dust samples can be sent to commercial laboratories for analysis of mouse allergen content, a good history focused on
sightings of mice or evidence of mice and general knowledge of mouse infestation in the community can be helpful in identifying
children who are likely to be exposed.
Significant exposure reduction can be achieved by eradication of infestation
Setting traps
Thorough inspection to identify holes and cracks, sealing of holes and cracks with copper mesh and caulk
Meticulous cleaning of kitchen and dining areas after food consumption
Storage of foods in chew-proof, sealed containers
Professionally applied rodenticide, if needed
Additional measures that may help reduce home mouse allergen exposure include:
NIH-PA Author Manuscript
Washing all bed linens in hot water every 2 weeks
Use of allergen-proof mattress and pillow encasements
HEPA purifiers
NIH-PA Author Manuscript
Curr Allergy Asthma Rep. Author manuscript; available in PMC 2014 December 01.
Anda mungkin juga menyukai
- ASTHMADokumen17 halamanASTHMAvinda astri permatasariBelum ada peringkat
- WHO MHGap Guide English PDFDokumen121 halamanWHO MHGap Guide English PDFYolanda Dwi OktaviyaniBelum ada peringkat
- Adsorbents and Adsorption Processes For Pollution ControlDokumen30 halamanAdsorbents and Adsorption Processes For Pollution ControlJoao MinhoBelum ada peringkat
- Procedure FireDokumen28 halamanProcedure FireRichard D DuBelum ada peringkat
- Bhert - EoDokumen2 halamanBhert - EoRose Mae LambanecioBelum ada peringkat
- Autoimmune ReviewDokumen11 halamanAutoimmune ReviewPM100% (1)
- MHGap Intervention Guide PDFDokumen107 halamanMHGap Intervention Guide PDFfundj22100% (1)
- MHGap Intervention Guide PDFDokumen107 halamanMHGap Intervention Guide PDFfundj22100% (1)
- MHGap Intervention Guide PDFDokumen107 halamanMHGap Intervention Guide PDFfundj22100% (1)
- MHGap Intervention Guide PDFDokumen107 halamanMHGap Intervention Guide PDFfundj22100% (1)
- Will The Real Inner-City Allergen Please Stand Up?: EditorialDokumen2 halamanWill The Real Inner-City Allergen Please Stand Up?: EditorialPratita Jati PermatasariBelum ada peringkat
- Asthma and Its Environmental Triggers 508Dokumen2 halamanAsthma and Its Environmental Triggers 508SaiKai54Belum ada peringkat
- Annotated Journal Article 1Dokumen9 halamanAnnotated Journal Article 1aamontesinosmBelum ada peringkat
- 436 2010 Article 2064Dokumen6 halaman436 2010 Article 2064Arif SetiawanBelum ada peringkat
- Clinico - Seroepidemiological Evaluation of Toxocariasis in Asthmatic Pediatric Children in Mansoura City in EgyptDokumen5 halamanClinico - Seroepidemiological Evaluation of Toxocariasis in Asthmatic Pediatric Children in Mansoura City in EgyptInternational Medical PublisherBelum ada peringkat
- Animals-09-01015 Regresion Arbol ParasitosDokumen13 halamanAnimals-09-01015 Regresion Arbol ParasitosJesús PeñaBelum ada peringkat
- AfricaDokumen12 halamanAfricaBrandon AlvarezBelum ada peringkat
- Environmental and Occupational AllergiesDokumen11 halamanEnvironmental and Occupational AllergiesRatna WindyaningrumBelum ada peringkat
- Rol de Las Aves en Epidemiología en Transmisión de ZoonosisDokumen21 halamanRol de Las Aves en Epidemiología en Transmisión de ZoonosissandraBelum ada peringkat
- Revised RRLDokumen5 halamanRevised RRLJoshua ArcairaBelum ada peringkat
- New England Journal Medicine: The ofDokumen11 halamanNew England Journal Medicine: The ofchemptnkBelum ada peringkat
- International Journal of EpidemiologyDokumen9 halamanInternational Journal of Epidemiologycooky maknaeBelum ada peringkat
- Management of Acute Respiratory Diseases PDFDokumen21 halamanManagement of Acute Respiratory Diseases PDFFernandoXavierBelum ada peringkat
- Wild Great Apes As Sentinels and Sources of Infectious DiseaseDokumen8 halamanWild Great Apes As Sentinels and Sources of Infectious Diseaseapi-286454950Belum ada peringkat
- Arthropod Allergens in Urban Homes: Ljerka PRESTERDokumen10 halamanArthropod Allergens in Urban Homes: Ljerka PRESTERname_LeaBelum ada peringkat
- Parasites That Heal: What Our Old Friends' Can Do For Us - Integrative Health EducationDokumen3 halamanParasites That Heal: What Our Old Friends' Can Do For Us - Integrative Health EducationmayapetrovaBelum ada peringkat
- Investigation of The Hygiene Hypothesis: Current Issues and Future DirectionsDokumen3 halamanInvestigation of The Hygiene Hypothesis: Current Issues and Future DirectionsAimee FBelum ada peringkat
- Review of Related LiteratureDokumen11 halamanReview of Related LiteratureLunel John RuazaBelum ada peringkat
- Immunopathology of Dirofilaria Immitis InfectionDokumen11 halamanImmunopathology of Dirofilaria Immitis InfectionrodrigocpnovaisBelum ada peringkat
- Mice ResearchDokumen7 halamanMice Researchedione quinonesBelum ada peringkat
- En 14Dokumen8 halamanEn 14buo_souzaBelum ada peringkat
- Clinico - Seroepidemiological Evaluation of Toxocariasis in Asthmatic Pediatric Children in Mansoura City in EgyptDokumen5 halamanClinico - Seroepidemiological Evaluation of Toxocariasis in Asthmatic Pediatric Children in Mansoura City in EgyptInternational Medical PublisherBelum ada peringkat
- Wilson Et Al 2012 Allergic Sensitization Through The Airway Primes th17 Dependent Neutrophilia and AirwayDokumen11 halamanWilson Et Al 2012 Allergic Sensitization Through The Airway Primes th17 Dependent Neutrophilia and AirwaytempeuedanBelum ada peringkat
- Rhinitis AlergiDokumen4 halamanRhinitis AlergipicassowaffleBelum ada peringkat
- House Dust Mite and Cockroach Exposure Are Strong Risk Factors For Positive Allergy Skin Test Responses in The Childhood Asthma Management ProgramDokumen7 halamanHouse Dust Mite and Cockroach Exposure Are Strong Risk Factors For Positive Allergy Skin Test Responses in The Childhood Asthma Management ProgramJacqueline HaroBelum ada peringkat
- The Global Status of Dirofilaria Immitis in Dogs - A Systematic Review and Metaanalysis Based On Published ArticlesDokumen13 halamanThe Global Status of Dirofilaria Immitis in Dogs - A Systematic Review and Metaanalysis Based On Published Articlesyudhi arjentiniaBelum ada peringkat
- 2623 FullDokumen2 halaman2623 FullNefri ArshintaBelum ada peringkat
- Indoor Mold Exposure: Epidemiology, Consequences and ImmunothapyDokumen15 halamanIndoor Mold Exposure: Epidemiology, Consequences and ImmunothapyAtlas CerboBelum ada peringkat
- Literature of AsthmaDokumen23 halamanLiterature of AsthmaAbrar Hendri PutraBelum ada peringkat
- Finland, 2015, Iguanas Con Niños.Dokumen3 halamanFinland, 2015, Iguanas Con Niños.Javier Zuñiga AguilarBelum ada peringkat
- Congenic Mice: Cutting Tools For Complex Immune Disorders: Ute C. Rogner and Philip AvnerDokumen11 halamanCongenic Mice: Cutting Tools For Complex Immune Disorders: Ute C. Rogner and Philip AvnerJimit GandhiBelum ada peringkat
- Arizmendi 2011Dokumen10 halamanArizmendi 2011TifanyNabilahBelum ada peringkat
- AsthmaDokumen118 halamanAsthmaDaroo D.TBelum ada peringkat
- Diette Et Al. (2007) - Home Indoor Pollutant Exposures Among Inner-City Children With and Without AsthmaDokumen5 halamanDiette Et Al. (2007) - Home Indoor Pollutant Exposures Among Inner-City Children With and Without AsthmanimaaandmBelum ada peringkat
- Possible Role of Songbirds and Parakeets in Transmission of Influenza A (H7N9) Virus To HumansDokumen6 halamanPossible Role of Songbirds and Parakeets in Transmission of Influenza A (H7N9) Virus To Humansapi-102069217Belum ada peringkat
- An Understanding of The Genetic Basis of Asthma: Review ArticleDokumen13 halamanAn Understanding of The Genetic Basis of Asthma: Review ArticlerastiooBelum ada peringkat
- Household Pet Exposure, Allergic Sensitization, and Rhinitis in The U.S. PopulationDokumen7 halamanHousehold Pet Exposure, Allergic Sensitization, and Rhinitis in The U.S. PopulationWildan TrianaBelum ada peringkat
- Etm 12 04 2383Dokumen4 halamanEtm 12 04 2383mukhlis akmalBelum ada peringkat
- Do Levels of Airborne Grass Pollen InfluDokumen7 halamanDo Levels of Airborne Grass Pollen InfluandalucistasBelum ada peringkat
- Infl de Los Diferentes Tipos de Material de Cama en La Prevalencia de PododermatitisDokumen24 halamanInfl de Los Diferentes Tipos de Material de Cama en La Prevalencia de PododermatitisLoreto Rojas PeraltaBelum ada peringkat
- Number 1Dokumen3 halamanNumber 1Michael HostiadiBelum ada peringkat
- NIH Public Access: Author ManuscriptDokumen20 halamanNIH Public Access: Author ManuscriptteacherferhdzBelum ada peringkat
- Kennedy 2007Dokumen8 halamanKennedy 2007Sílvia BastosBelum ada peringkat
- Epidimiology Chapter 4Dokumen24 halamanEpidimiology Chapter 4Sarika YadavBelum ada peringkat
- Prevelance of e Coli in Poultry FarmDokumen102 halamanPrevelance of e Coli in Poultry FarmFavour ChukwuelesieBelum ada peringkat
- Association Between Domestic Mould and Mould Components, and Asthma and Allergy in Children: A Systematic ReviewDokumen13 halamanAssociation Between Domestic Mould and Mould Components, and Asthma and Allergy in Children: A Systematic ReviewYehezkiel JonathanBelum ada peringkat
- 7 MRSA and Controling-12Dokumen12 halaman7 MRSA and Controling-12RavinderenPichanBelum ada peringkat
- Review of Mouse Models Applied To The Study of AsthmaDokumen10 halamanReview of Mouse Models Applied To The Study of AsthmayuriBelum ada peringkat
- Science of The Total EnvironmentDokumen11 halamanScience of The Total EnvironmentVita MeščeriakovaBelum ada peringkat
- Bosholn Et Al. 2019Dokumen12 halamanBosholn Et Al. 2019marianeBelum ada peringkat
- Research Paper Final DraftDokumen9 halamanResearch Paper Final Draftapi-605105565Belum ada peringkat
- Intestinal HelminthsDokumen4 halamanIntestinal HelminthssivaBelum ada peringkat
- Eeckey Honors Paper 2Dokumen7 halamanEeckey Honors Paper 2api-668378939Belum ada peringkat
- International Journal For Parasitology: Drugs and Drug ResistanceDokumen10 halamanInternational Journal For Parasitology: Drugs and Drug ResistanceWillow MariamBelum ada peringkat
- Harrison2003laws of AomDokumen27 halamanHarrison2003laws of Aom211097salBelum ada peringkat
- Torgerson 2003Dokumen16 halamanTorgerson 2003Eryc Luan DiasBelum ada peringkat
- Asthma: Whom Does It Affect?Dokumen11 halamanAsthma: Whom Does It Affect?Ken KennyBelum ada peringkat
- Caged Birds as a Source of CNSLD, Lung Cancer and Other Human DiseasesDari EverandCaged Birds as a Source of CNSLD, Lung Cancer and Other Human DiseasesBelum ada peringkat
- Insect ImmunologyDari EverandInsect ImmunologyNancy E. BeckageBelum ada peringkat
- Iron - The TestDokumen3 halamanIron - The TestResti Zulvanita DeviBelum ada peringkat
- Genitourinary System 1Dokumen35 halamanGenitourinary System 1NofiWulandariBelum ada peringkat
- Microorganism On Cardiovascular: Sy. Miftah El JannahDokumen22 halamanMicroorganism On Cardiovascular: Sy. Miftah El JannahResti Zulvanita DeviBelum ada peringkat
- Blood TransfusionDokumen2 halamanBlood TransfusionAlbano HallBelum ada peringkat
- Patologi Anatomi: Gastro EnterologiDokumen31 halamanPatologi Anatomi: Gastro EnterologiResti Zulvanita DeviBelum ada peringkat
- BMI AnakDokumen8 halamanBMI AnakResti Zulvanita DeviBelum ada peringkat
- WJCC 2 859Dokumen8 halamanWJCC 2 859Resti Zulvanita DeviBelum ada peringkat
- ManajemenDokumen31 halamanManajemenResti Zulvanita DeviBelum ada peringkat
- ManajemenDokumen31 halamanManajemenResti Zulvanita DeviBelum ada peringkat
- Medical Tests TIBCDokumen2 halamanMedical Tests TIBCResti Zulvanita DeviBelum ada peringkat
- Kuliah RCCDokumen17 halamanKuliah RCCResti Zulvanita DeviBelum ada peringkat
- Spectrum and Management CLDDokumen91 halamanSpectrum and Management CLDResti Zulvanita DeviBelum ada peringkat
- MEDICAL REVIEW Tumor Wilms NephroblastomaDokumen8 halamanMEDICAL REVIEW Tumor Wilms NephroblastomanadilapadBelum ada peringkat
- 08 - GlaucomaDokumen80 halaman08 - GlaucomaabcdshBelum ada peringkat
- Bakteri Anaerob: Morfologi, Fisiologi, Epidemiologi, Diagnosis, Pemeriksaan Sy. Miftahul El J.TDokumen46 halamanBakteri Anaerob: Morfologi, Fisiologi, Epidemiologi, Diagnosis, Pemeriksaan Sy. Miftahul El J.TResti Zulvanita DeviBelum ada peringkat
- MEDICAL REVIEW Tumor Wilms NephroblastomaDokumen8 halamanMEDICAL REVIEW Tumor Wilms NephroblastomanadilapadBelum ada peringkat
- Pemeriksaan Psikiatri 2010Dokumen71 halamanPemeriksaan Psikiatri 2010Resti Zulvanita DeviBelum ada peringkat
- RefraksiDokumen53 halamanRefraksigilaliBelum ada peringkat
- Lapjag 11-17 FADDokumen12 halamanLapjag 11-17 FADResti Zulvanita DeviBelum ada peringkat
- RefraksiDokumen53 halamanRefraksigilaliBelum ada peringkat
- RefraksiDokumen53 halamanRefraksigilaliBelum ada peringkat
- Ni Hms 545265Dokumen21 halamanNi Hms 545265Resti Zulvanita DeviBelum ada peringkat
- Higher Algebra - Hall & KnightDokumen593 halamanHigher Algebra - Hall & KnightRam Gollamudi100% (2)
- Cargador de BateríaDokumen34 halamanCargador de BateríaBenBelum ada peringkat
- Review - Practical Accounting 1Dokumen2 halamanReview - Practical Accounting 1Kath LeynesBelum ada peringkat
- Inlet Manifold Pressure - Test: Testing and AdjustingDokumen2 halamanInlet Manifold Pressure - Test: Testing and AdjustingAbdoulaye Boua BERTHEBelum ada peringkat
- Chemistry Xi: Short Questions and 20% Long QuestionsDokumen3 halamanChemistry Xi: Short Questions and 20% Long QuestionsSyed Nabeel HassanBelum ada peringkat
- DT 2107Dokumen1 halamanDT 2107Richard PeriyanayagamBelum ada peringkat
- FINAL PAPER Marketing Plan For Rainbow Air PurifierDokumen12 halamanFINAL PAPER Marketing Plan For Rainbow Air PurifierMohola Tebello Griffith100% (1)
- Adenoid HypertrophyDokumen56 halamanAdenoid HypertrophyWidi Yuli HariantoBelum ada peringkat
- A Comprehensive Review of Cementitious Grouts - Composition, Properties, Requirements and Advanced PerformanceDokumen16 halamanA Comprehensive Review of Cementitious Grouts - Composition, Properties, Requirements and Advanced PerformanceiporrasBelum ada peringkat
- Gender, Slum Poverty and Climate Change in Flooded River Lines in Metro ManilaDokumen53 halamanGender, Slum Poverty and Climate Change in Flooded River Lines in Metro ManilaADBGADBelum ada peringkat
- Big 9 Master SoalDokumen6 halamanBig 9 Master Soallilik masrukhahBelum ada peringkat
- TC 10 emDokumen7 halamanTC 10 emDina LydaBelum ada peringkat
- PMI Framework Processes PresentationDokumen17 halamanPMI Framework Processes PresentationAakash BhatiaBelum ada peringkat
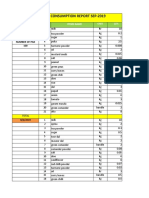
- Daily Staff Food Consumption Reports Sep-2019Dokumen4 halamanDaily Staff Food Consumption Reports Sep-2019Manjit RawatBelum ada peringkat
- Castle 1-3K E ManualDokumen26 halamanCastle 1-3K E ManualShami MudunkotuwaBelum ada peringkat
- ACF5950 - Assignment # 7 Semester 2 2015: The Business Has The Following Opening Balances: Additional InformationDokumen2 halamanACF5950 - Assignment # 7 Semester 2 2015: The Business Has The Following Opening Balances: Additional InformationkietBelum ada peringkat
- ReliabilityDokumen5 halamanReliabilityArmajaya Fajar SuhardimanBelum ada peringkat
- Neurocisticercosis PDFDokumen7 halamanNeurocisticercosis PDFFiorella Alexandra HRBelum ada peringkat
- EP500 Standard Electropneumatic Positioner: Installation and Maintenance InstructionsDokumen28 halamanEP500 Standard Electropneumatic Positioner: Installation and Maintenance InstructionsAlan ValdezBelum ada peringkat
- S ELITE Nina Authors Certain Ivey This Reproduce Western Material Management Gupta Names Do OntarioDokumen15 halamanS ELITE Nina Authors Certain Ivey This Reproduce Western Material Management Gupta Names Do Ontariocarlos menaBelum ada peringkat
- Acute Renal Failure in The Intensive Care Unit: Steven D. Weisbord, M.D., M.Sc. and Paul M. Palevsky, M.DDokumen12 halamanAcute Renal Failure in The Intensive Care Unit: Steven D. Weisbord, M.D., M.Sc. and Paul M. Palevsky, M.Dkerm6991Belum ada peringkat
- Demages Goods RecordDokumen22 halamanDemages Goods Recordtariq malikBelum ada peringkat
- AtelectasisDokumen37 halamanAtelectasisSandara ParkBelum ada peringkat
- Study Notes On Isomers and Alkyl HalidesDokumen3 halamanStudy Notes On Isomers and Alkyl HalidesChristian Josef AvelinoBelum ada peringkat
- Flame Retardant and Fire Resistant Cable - NexansDokumen2 halamanFlame Retardant and Fire Resistant Cable - NexansprseBelum ada peringkat
- Exercises - Fluid MechanicsDokumen3 halamanExercises - Fluid MechanicsgemnikkicBelum ada peringkat
- Xi 3 1Dokumen1 halamanXi 3 1Krishnan KozhumamBelum ada peringkat
- HVAC (Heating, Ventilation and Air Conditioning) : SRS PrecautionsDokumen1 halamanHVAC (Heating, Ventilation and Air Conditioning) : SRS PrecautionssoftallBelum ada peringkat