Bahan Referat Putri
Diunggah oleh
Putri MiraaJudul Asli
Hak Cipta
Format Tersedia
Bagikan dokumen Ini
Apakah menurut Anda dokumen ini bermanfaat?
Apakah konten ini tidak pantas?
Laporkan Dokumen IniHak Cipta:
Format Tersedia
Bahan Referat Putri
Diunggah oleh
Putri MiraaHak Cipta:
Format Tersedia
Supporting therapy pada critical ill secara umum
Oksigen merupakan salah satu pengobatan dalam emergensi yang secara umum digunakan
terutama pada keadaan hipoksemia yang tak diragukan lagi dapat menyelamatkan kehidupan.
Dipercaya secara luas bahwa pemberian oksigen dapat mengurangi dispnea pada keadaan
hipoksemia (rendah level oksigen di arteri). Dispnea dapat terjadi karena berbagai hal baik itu
karena penyakit kardiovaskuler hingga penyakit metabolik seperti asidosis metabolik.
Source: Kane B, Decalmer S, ODriscoll R. Emergency oxygen therapy: from guideline to
implementation. J European Respiratory Society. June 2013; 9(4).
Keadaan hipoksemia sangat mematikan dan harus segera diatasi. Pada sebagian besar pasien,
pemberian oksigen konsentrasi tinggi diperlukan dengan tujuan untuk memaksimalkan
konsentrasi oksigen inspirasi (FiO2). Kadar FiO2 bergantung pada ventilasi per menit dan laju
oksigen yang diberikan. Pasien dengan respiratory distress mempunyai ventilasi 30 liter/menit
dan pada keadaan tersebut pemberian face mask dengan laju oksigen 12 liter/menit hanya akan
menyediakan FiO2 sebesar 50%. Salah satu cara yang dapat digunakan untuk memperoleh FiO2
yang lebih tinggi adalah dengan menggunakan mask dengan reservoir bag (non-rebreathing
mask).
Jika diperkirakan terjadi syok sirkulasi maka pikirkan untuk melakukan fluid challenge.
Pemberian cairan secara cepat, misalnya dalam 10-15 menit berikan cairan kristalloid 250 ml
atau dengan pemberian cairan koloid dengan volume yang sama. Efek pemberian fluid challenge
dapat dipantau melalui tekanan darah, nadi, perfusi perifer, outpout urin, maupun tingkat
kesadarann.
Source: British Journal of Hospital Medicine. October 2007: 68 (10)
Manjemen pemberian cairan mempunyai pengaruh terutama pada durasi, keparahan
maupun outcome dari critical illness
Fluid management has a major impact on the duration, severity and outcome of critical
illness. Aggressive volume expansion to support tissue oxygen delivery as part of early goaldirected resuscitation algorithms for
shockespecially septic shockhas been associated with
dramatic improvements in outcome. Intravenous administration of extra fluid to top-up the
circulation increases cardiac output by the FrankStarling relationship. Again, Ernest Starling
described the key physiology we
still use today at every bed space based on observations of
isolated perfused dog hearts. He described the increase in
stroke volume seen with increased left ventricular stretch
[19, 20]. The result is that fluid administration increases
cardiac output, tissue blood flow and oxygen delivery to vital
organs (unless the heart is already failing). These core observations are translated into the
current recommendations for
haemodynamic support in septic shock in children. Consensus
guidance recommends administering bolus aliquots of
20 ml/kg very rapidly (up to 60 ml/kg in 15 min). The
volume given is titrated to observable indicators of adequate
organ perfusion. These include capillary refill time, conscious
level and urine output. In shock states, we have to reestablish tissue perfusion rapidly
without overdosing into
potentially harmful states of increased interstitial fluid. Numerous animal studies have
supported either crystalloid or
colloid as preferable for resuscitation in various species with
various aetiologies of shock. While the results of numerous studies of artificial colloids
have suggested minor effects on the times to shock reversal.
in comparison to crystalloids, the effect are largely small
and short-lived. There are indications of an increased risk of
AKI, especially with hydroxyethyl starches (HES). To summarise these datathe choice
between crystalloid
and colloid in septic shock is still open with some data in
favour of each [86, 87]. Starch-based solutions should probably be avoided. As early as
1932, Hartmann showed that normal saline
causes acidosis in children [90]. Much later, Ringers lactate
was shown to cause a decrease in osmolality [91].
Although studies have looked at the most appropriate
fluid for maintenance, no clear guidance is available in this
regard other than the caution on hypotonic solutions [92]. At
our hospital, we use isotonic solutions for maintenance with
close monitoring of electrolyte parameters
Source: Raman S, Peters MJ. Fluid management in the critically ill child. Pediatric Nephrology.
January 2013
Anda mungkin juga menyukai
- Promkes DiareDokumen10 halamanPromkes DiarePutri Miraa100% (3)
- Dislokasi Hip PosteriorDokumen12 halamanDislokasi Hip PosteriorPutri MiraaBelum ada peringkat
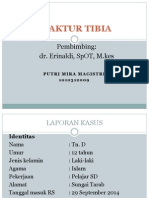
- Fraktur TibiaDokumen16 halamanFraktur TibiaPutri MiraaBelum ada peringkat
- Jurnal ProfDokumen21 halamanJurnal ProfPutri MiraaBelum ada peringkat
- Telur AsinDokumen18 halamanTelur AsinPutri Miraa0% (1)