Status Pasien
Diunggah oleh
Fajar Al-HabibiHak Cipta
Format Tersedia
Bagikan dokumen Ini
Apakah menurut Anda dokumen ini bermanfaat?
Apakah konten ini tidak pantas?
Laporkan Dokumen IniHak Cipta:
Format Tersedia
Status Pasien
Diunggah oleh
Fajar Al-HabibiHak Cipta:
Format Tersedia
Case Report
ORCHITIS DEXTRA
OLEH:
FAJAR AL-HABIBI
RSUD ABDOEL MOELOEK BANDAR LAMPUNG
MARET 2013
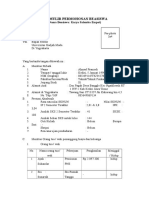
STATUS PASIEN
I. IDENTITAS PASIEN
Nama
: Tn. S
Umur
: 31 Tahun
Jenis kelamin
: Laki-laki
Pekerjaan
: Petani
Alamat
Suku
: Kecamatan Ketahun, Kabupaten Bengkulu Utara
: Jawa
Agama
Masuk RS : 10 Desember 2015
: Islam
II. ANAMNESA
Diambil dari autoanamnesa tanggal 10 Desember 2015
Keluhan utama
: benjolan pada kantung kemaluan sebelah kanan
Keluhan tambahan
: nyeri pada benjolan (+), mual (+), muntah (+),
Riwayat Penyakit Sekarang
Pasien datang dengan keluhan benjolan pada kantung kemaluan sejak tujuh
hari yang lalu (3 Desember 2015). Keluhan lainnya pasien merasa nyeri pada
benjolan, perut terasa mual dan muntah 3x/hari. Kantung kemaluan dirasakan
membesar dan membenjol disertai demam selama dua hari. Kemudian pasien
memeriksakan dirinya ke dokter terdekat di daerahnya dan pasien diberikan
terapi oleh dokter tersebut. Pasien lupa dengan jenis obat yang diberikan oleh
dokter tersebut. Setelah diberikan terapi selaama tiga hari keluhan demam
berkurang sampai hilang, benjolan membesar berkurang. Karena merasa
benjolan masih ada, pasien memeriksakan diri ke dokter di RS Bhayangkara
yang ada di kota bengkulu. Dan dilakukan pemeriksaan darah yang hasilnya
normal. Pasien disarankan k RS DKT untuk konsultasi pada dokter bedah
terkait benjolan di kemaluannya.
Riwayat Penyakit Keluarga
Tidak ada anggota keluarga yang mengalami sakit seperti ini.
Riwayat Masa Lampau
Trauma terdahulu
: Tidak ada
Operasi
: Tidak ada
Sistem Saraf
: Tidak ada
Sistem Kardiovaskular
: Tidak ada
Sistem Gastrointestinal
: Tidak ada
Sistem Urinarius
: Tidak ada
Sistem Genitalis
: Tidak ada
Sistem Muskuloskeletal : Tidak ada
III. STATUS PRESENT
STATUS UMUM (16 maret 2013)
Keadaan umum
: baik
Kesadaran
: Compos mentis
Keadaan Gizi
: baik
Kulit
: Turgor normal
PEMERIKSAAN FISIK (16 Maret 2013)
TANDA VITAL
Tekanan darah
: 120/70 mmHg
Nadi
: 80 x/menit
Pernafasan
: 32 x/menit
Suhu
: 37 oC
Kepala dan Muka
Bentuk
: Normocephalic
Mata
: terdapat luka lecet di palpebra sinistra
Konjungtiva tidak pucat
Sklera anikterik
Pupil bulat sentral isokor
Reflek cahaya (+/+)
Telinga
Hidung
: Septum tidak deviasi, konka tidak hipertropi.
Tenggorokan
: deviasi trakea (-), pembesaran kelenjar tiroid (-),
: Liang lapang, serumen telinga kiri dan kanan (+).
Bruit a. Carotis (-)
Mulut
: Bibir tidak kering, lidah tidak kotor, sianosis (-)
Gigi
: Caries (-)
KGB
: Tidak teraba pembesaran
Tiroid
: Tidak teraba pembesaran
JVP
: Tidak tampak peningkatan
Leher
Thoraks
1. Paru-Paru
Inspeksi
: Bentuk dada simetris, pergerakan hemitoraks kiri
dan kanan simetris
Palpasi
: Fremitus taktil hemitoraks kiri dan kanan simetris
Perkusi
: Sonor, batas paru hati sela iga VI garis mid
clavicula kanan
Auskultasi
: Vesikular pada paru kiri dan kanan
ronkhi dan wheezing tidak ada
2. Jantung
Inspeksi
: Iktus kordis tidak terlihat
Palpasi
: Iktus kordis teraba pada sela iga V linea mid
clavicula kiri
Perkusi
: Batas atas sela iga II parasternal kiri
Batas kanan sela iga IV midsternal kanan
Batas kiri sela iga V midclavicula kiri
Auskultasi
: Bunyi jantung I II reguler, murmur (-), gallop (-)
Abdomen
-
Inspeksi
: Perut datar dan tidak tampak penonjolan massa
Palpasi
: Hepar dan lien tidak teraba pembesaran
Perkusi
: Timpani
Auskultasi
: Bising usus (+) normal
Ekstremitas
-
Superior
: oedem (-), sianosis (-)
Inferior
: oedem (-), sianosis (-)
Genitalia Eksterna
Tidak terpasang kateter
Transluminasi skrotum dekstra (-), pada sinistra tidak dilakukan karena
masih terdapat luka yang cukup erosif.
Skrotum sinistra lebih besar dengan penampakan ulkus erosif yang
mengeluarkan banyak pus. Luas area di skrotum yang terdapat luka 25
cm2. Tampak lapisan-lapisan kulit yang telah nekrosis pada daerah luka.
Sensibilitas (+/+)
STATUS LOKALIS
IV. PEMERIKSAAN PENUNJANG
1. Darah (14 Maret 2013)
Hb
: 10 gr/dl
(N laki-laki= 13,5-18 gr/dl)
Hematokrit
: 31%
(N laki-laki= 40-54%)
LED
: 48 mm/jam
(N laki-laki= 0-10 mm/jam)
Trombosit
: 448.000/ul
(N= 150.000-400.000/ul)
Leukosit
:11.100/ul
(N= 4500-10.700/ul)
Hitung jenis
Basofil
(N)
:0%
( 0-1% )
Eosinofil
: 1%
(1-3%)
Netrofil batang
:1%
( 2-6% )
Netrofil segmen
: 82 %
( 50-70% )
Limfosit
: 9%
( 20-40% )
Monosit
: 7%
( 2-8% )
2. Kimia Darah (16 Maret 2013)
Total protein : 5,5 g/dl
(N= 6.0 - 8,6 g/dl)
Albumin
: 2,0 g/dl
(N= 3,5 - 5,0 g/dl)
Globulin
: 3,5 g/dl
(N= 2,3 - 3,5 g/dl)
Ureum
: 73 mg/dl
(N laki-laki= 10 - 40 mg/dl)
Creatinine
: 0,7 mg/dl
(N laki-laki= 0,7 - 1,3 mg/dl)
Natrium
: 135 mmol/L (N= 135 - 180 mmol/L)
Kalium
Calsium
Clorida
:3,6 mmol/L
: 7,5 mg/dl
(N= 3,5 - 5,5 mmol/L)
(N= 8,8 - 10,5 mg/dl)
: 100 mmol/L (N= 98 - 110 mmol/L)
3. Kultur Pus Dan Uji Sensitivitas Antibiotik
a. 14 Maret 2013-03-23
Hasil kultur: ditemukan bakteri gram negatif (Proteus sp.)
Angka kuman 150 x 103 bakteri/ml
Hasil uji sensitivitas:
b. 16 Maret 2013
Hasil kultur: ditemukan bakteri gram negatif (Klebsiella sp.)
Hasil uji sensitivitas:
RESUME
Laki-laki-usia 39 tahun dengan keluhan skrotum terasa nyeri, panas, bernanah dan
berdarah banyak. Riwayat penyakit sekarang pasien mengalami kecelakaan jatuh
dari motor. Pasien mengalami trauma pada perut bagian bawah dan luka lecet
pada mata kiri. Tiga hari berikutnya, pasien mengeluhkan pembesaran pada
skrotum sinistra. Skrotum terasa panas dan nyeri. Esoknya, pada skrotum pasien
keluar nanah dan darah yang banyak. Skrotum sinistra lebih besar dengan
penampakan ulkus erosif yang mengeluarkan banyak pus. Luas area di skrotum
yang terdapat luka 25 cm2. Tampak lapisan-lapisan kulit yang telah nekrosis
pada daerah luka.
10
Diagnosis Banding
Cellulitis
Emergent Management of Acute Epididymitis
Emergent Management of Necrotizing Fasciitis
Gas Gangrene in Emergency Medicine
Hernias
Hydrocele sinistra in Emergency Medicine
Orchitis
Testicular Torsion in Emergency Medicine
Diagnosis Kerja
Fourniers gangrene
Penatalaksanaan
-
Debridement yang adekuat. Pada kasus ini setiap hari daerah luka dibersihkan
dengan menyemprotkan larutan fisiologis NaCl 0,9%.
Antibiotika. Pada saat sebelum dikultur pasien diberikan ciprofloxaxin 500 mg
melalui intravena dua kali sehari. Setelah dilakukan uji sensitifitas didapatkan
antibiotik yang masih sensitif adalah meropenem kemudian kepada pasien
diberikan terapi meropenem dengan dosis 500 mg per intravena dua kali
sehari.
Prognosa
Fourniers gangrene severity index (FGSI), sampai 16 Maret 2013
Temperature
Heart rate
Respiration rate
Serum sodium
Serum potassium
Serum creatinine
:0
:0
:0
:0
:0
:0
11
Packed cell volum (%): 0
Whole blood cell count: 0
Serum bicarbonate : ?
FGSI= 0-4,
Body Surface Area (BSA)= 25 cm2
Quo ad Vitam (hidup): dubia ad Bonam
Quo ad Functionam (fungsi) : dubia ad Bonam
Quo ad Sanationam (sembuh): dubia ad Bonam
TINJAUAN KEPUSTAKAAN
1, anatomi
12
PATHOGENESIS
Fournier's gangrene (FG) is a fulminant form of polymicrobial necrotising fascitis
of the perineal, genital, or perianal regions. Impaired immunity is important for
increasing susceptibility to Fournier gangrene. Trauma to the genitalia is a
frequently recognized vector for the introduction of bacteria that initiate the
infectious process.
PATHOPHYSIOLOGY
Infection of superficial perineal fascia (Colles fascia) may spread to the penis and
scrotum via Buck and dartos fascia, or to the anterior abdominal wall via Scarpa
fascia, or vice versa. Colles fascia is attached to the perineal body and urogenital
diaphragm posteriorly and to the pubic rami laterally, thus limiting progression in
these directions. Testicular involvement is rare, as the testicular arteries originate
directly from the aorta and thus have a blood supply separate from the affected
region.
13
Microorganism virulence results from the production of toxins or enzymes that
create an environment conducive to rapid microbial multiplication. Although
Meleney in 1924 attributed the necrotizing infections to streptococcal species
only, subsequent clinical series have emphasized the multiorganism nature of most
cases of necrotizing infection, including Fournier gangrene.
Most authorities believe that polymicrobial involvement is necessary to create the
synergy of enzyme production that promotes rapid multiplication and spread of
Fournier gangrene. For example, one microorganism might produce the enzymes
necessary to cause coagulation of the nutrient vessels. Thrombosis of these
nutrient vessels reduces local blood supply; thus, tissue oxygen tension falls.
The resultant tissue hypoxia allows growth of facultative anaerobes and
microaerophilic organisms. These latter microorganisms, in turn, may produce
enzymes (eg, lecithinase, collagenase), which lead to digestion of fascial barriers,
thus fueling the rapid extension of the infection.
Fascial necrosis and digestion are hallmarks of this disease process; this is
important to appreciate because it provides the surgeon with a clinical marker of
the extent of tissue involvement. Specifically, if the fascial plane can be separated
easily from the surrounding tissue by blunt dissection, it is quite likely to be
involved with the ischemic-infectious process; therefore, any such dissected tissue
should be excised.
DIAGNOSIS
Anamnesis
The clinical course usually progresses through the following phases:
1. Prodromal symptoms of fever and lethargy, which may be present for 2-7
days
14
2. Intense genital pain and tenderness that is usually associated with edema
of the overlying skin; pruritus may also be present
3. Increasing genital pain and tenderness with progressive erythema of the
overlying skin
4. Dusky appearance of the overlying skin; subcutaneous crepitation
5. Obvious gangrene of a portion of the genitalia; purulent drainage from
wounds
Physical Examination
The physician should direct particular attention to palpation of the genitalia and
perineum and to the digital rectal examination, to assess for signs of the disease
and to seek a potential portal of entry. Fluctuance, soft-tissue crepitation,
localizing tenderness, or occult wounds in any of these sites should alert the
examiner to possible Fournier disease.
Skin overlying the affected region may be normal, erythematous, edematous,
cyanotic, bronzed, indurated, blistered, and/or frankly gangrenous. Skin
appearance often underestimates the degree of underlying disease.
A feculent odor may be present secondary to infection with anaerobic bacteria.
Crepitus may be present, but its absence does not exclude the presence
ofClostridium species or other gas-producing organisms.
Systemic symptoms (eg, fever, tachycardia, hypotension) may be present.
Variables in Fournier's gangrene severity index (FGSI)
15
Pathologic evaluation of the involved tissue may reveal the following
pathognomonic findings of Fournier gangrene:
Necrosis of the superficial and deep fascial planes
Fibrinoid thrombosis of the nutrient arterioles
Polymorphonuclear cell infiltration
Microorganisms identified within the involved tissues
Fibrinoid thrombosis of the nutrient vessels that supply the superficial and deep
fascia is the finding that most commonly indicates Fournier disease. Widespread
necrosis of the fascia with acute inflammatory cell infiltration and necrotic debris
is frequently evident, as is the presence of causative microorganisms within the
tissues.
This extensive inflammatory process is frequently present deep to intact skin. The
skin itself is often minimally involved with the inflammatory process until late in
the disease.
16
THERAPY
Surgical diagnosis and debridement
Once a diagnosis of Fournier gangrene is established, all necrotic tissue must be
excised. In a large retrospective review of 379 patients, Sugihara et al confirmed
the opinion that early surgical intervention reduces mortality. Those who
underwent earlier intervention had a lower fatality rate (odds ratio, 0.38) than
those whose intervention was delayed to 3 days or later.
The skin should be opened widely to expose the full extent of the underlying
fascial and subcutaneous tissue necrosis. All fascial planes that separate easily
with blunt dissection should be considered involved and therefore excised. The
dissection should be carried out to include bleeding tissues ( tissue that is well
vascularized).
Send samples of excised tissue for aerobic and anaerobic cultures and a histologic
assessment.
17
Given the characteristic thrombosis of the nutrient vessels, the overlying skin has
impaired blood supply and should be excised if significantly undermined. The
authors strongly recommend radical excisional debridement (see below image)
with electrocautery in order to reduce the considerable operative blood loss if the
area of involvement is extensive.
Patient with Fournier gangrene following radical debridement. A dorsal slit was
made in the prepuce to expose the glans penis. Urethral catheterization was
performed. Incision into the point of maximal tenderness on the right side of the
perineum revealed gangrenous necrosis that involved the anterior and posterior
aspects of the perineum, the entirety of the right hemiscrotum, and the posterior
medial aspect of the right thigh. The skin and involved fascia were excised from
these areas. Reconstruction of this defect was performed in a staged approach. A
gracilis rotational muscle flap taken from the right thigh was used to fill the cavity
in the posterior right perineum as the first step. The remainder of the defect was
covered with split-thickness skin grafts. This patient made a full recovery.
The testicles are often spared in the necrotizing process. If it is uninvolved, place
the exposed testicle in a subcutaneous pocket to prevent desiccation. If a testicle is
involved in the necrotic process or its viability is questioned, performorchiectomy.
Antibiotic
The goals of pharmacotherapy in Fournier gangrene are to reduce morbidity and
to control the infection. Broad-spectrum antibiotics should be given early in
18
treatment. Tetanus prophylaxis is indicated if soft-tissue injury is present. Gold
therapy antibiotic at fournier gangren is based on culture purulent.
Treatment of Fournier gangrene involves the institution of broad-spectrum
antibiotic therapy. The antibiotic spectrum should cover staphylococci,
streptococci, the Enterobacteriaceae family of organisms, and anaerobes.
A reasonable empiric regimen might consist of ciprofloxacin and clindamycin.
Clindamycin is particularly useful in the treatment of necrotizing soft-tissue
infections because of its gram-positive and anaerobic spectrum of activity. In
animal models of streptococcal infection, clindamycin has been shown to yield
response rates superior to those of penicillin or erythromycin, even in the context
of delayed treatment.[47]
Other possible choices include ampicillin/sulbactam, ticarcillin/clavulanate, or
piperacillin/tazobactam
in
combination
with
an
aminoglycoside
and
metronidazole or clindamycin. Vancomycin can be used to provide coverage for
methicillin-resistant Staphylococcus aureus (MRSA).
In
cases
associated
with
sepsis
syndrome,
therapy
with
intravenous
immunoglobulin (IVIG), which is thought to neutralize superantigens (eg,
streptotoxins A and B) believed to mitigate the exaggerated cytokine response, has
been shown to be a good adjuvant to appropriate antibiotic coverage and complete
surgical debridement.[48]
Reconstruction
Once the infection is eradicated, healthy granulation tissue develops; this signifies
the time to proceed to reconstruction.
Options for reconstruction include the following:
Primary closure of the skin, if possible
Local skin flap coverage
Split-thickness skin grafts
19
Muscular flaps, which are used to fill a cavity (eg, ischiorectal space)
Anda mungkin juga menyukai
- Surat Pengalaman Kerja Fajar Al-HabibiDokumen1 halamanSurat Pengalaman Kerja Fajar Al-HabibiFajar Al-HabibiBelum ada peringkat
- Bab III RevisedDokumen7 halamanBab III RevisedFajar Al-HabibiBelum ada peringkat
- Pengunduran Diri PutriDokumen1 halamanPengunduran Diri PutriFajar Al-HabibiBelum ada peringkat
- Surat Keputusan Kepala Puskesmas Gunung Sari MaretDokumen5 halamanSurat Keputusan Kepala Puskesmas Gunung Sari MaretFajar Al-HabibiBelum ada peringkat
- Surat Rekom Atasan Untuk Sip DR - FajarDokumen1 halamanSurat Rekom Atasan Untuk Sip DR - FajarFajar Al-HabibiBelum ada peringkat
- CV Fajar Al-HabibiDokumen4 halamanCV Fajar Al-HabibiFajar Al-HabibiBelum ada peringkat
- Bab IvDokumen6 halamanBab IvFajar Al-HabibiBelum ada peringkat
- Bab II Super RevisedDokumen9 halamanBab II Super RevisedFajar Al-HabibiBelum ada peringkat
- Daftar PustakaDokumen4 halamanDaftar PustakaFajar Al-HabibiBelum ada peringkat
- Bab IDokumen5 halamanBab IFajar Al-HabibiBelum ada peringkat
- Bab IDokumen6 halamanBab IFajar Al-HabibiBelum ada peringkat
- Bab IvDokumen6 halamanBab IvFajar Al-HabibiBelum ada peringkat
- Daftar GambarDokumen2 halamanDaftar GambarAhmad IsmatullahBelum ada peringkat
- Daftar TabelDokumen1 halamanDaftar TabelFajar Al-HabibiBelum ada peringkat
- Halaman PersetujuanDokumen1 halamanHalaman PersetujuanFajar Al-HabibiBelum ada peringkat
- Bab II Super RevisedDokumen12 halamanBab II Super RevisedFajar Al-HabibiBelum ada peringkat
- Bab III RevisedDokumen8 halamanBab III RevisedFajar Al-HabibiBelum ada peringkat
- CoverDokumen1 halamanCoverFajar Al-HabibiBelum ada peringkat
- Daftar IsiDokumen2 halamanDaftar IsiFajar Al-HabibiBelum ada peringkat
- COVER HasilDokumen1 halamanCOVER HasilFajar Al-HabibiBelum ada peringkat
- Bab IvDokumen1 halamanBab IvFajar Al-HabibiBelum ada peringkat
- Bab VDokumen1 halamanBab VFajar Al-HabibiBelum ada peringkat
- Terjamahan Jurnal 1Dokumen18 halamanTerjamahan Jurnal 1Fajar Al-HabibiBelum ada peringkat
- Jenis MaduDokumen7 halamanJenis MaduFajar Al-HabibiBelum ada peringkat
- KTI Bab IIIDokumen2 halamanKTI Bab IIIFajar Al-HabibiBelum ada peringkat
- Ahmad PramudiDokumen4 halamanAhmad PramudiFajar Al-HabibiBelum ada peringkat
- COVERDokumen1 halamanCOVERFajar Al-HabibiBelum ada peringkat
- KTI Bab VDokumen1 halamanKTI Bab VFajar Al-HabibiBelum ada peringkat
- CovernolandaDokumen1 halamanCovernolandaFajar Al-HabibiBelum ada peringkat
- KTI Bab VDokumen1 halamanKTI Bab VFajar Al-HabibiBelum ada peringkat