Tutor 14 Okt 18
Diunggah oleh
Fajar Sutrisna0 penilaian0% menganggap dokumen ini bermanfaat (0 suara)
13 tayangan3 halamanJudul Asli
tutor 14 okt 18.docx
Hak Cipta
© © All Rights Reserved
Format Tersedia
DOCX, PDF, TXT atau baca online dari Scribd
Bagikan dokumen Ini
Apakah menurut Anda dokumen ini bermanfaat?
Apakah konten ini tidak pantas?
Laporkan Dokumen IniHak Cipta:
© All Rights Reserved
Format Tersedia
Unduh sebagai DOCX, PDF, TXT atau baca online dari Scribd
0 penilaian0% menganggap dokumen ini bermanfaat (0 suara)
13 tayangan3 halamanTutor 14 Okt 18
Diunggah oleh
Fajar SutrisnaHak Cipta:
© All Rights Reserved
Format Tersedia
Unduh sebagai DOCX, PDF, TXT atau baca online dari Scribd
Anda di halaman 1dari 3
Perdarahan antepartum adalah perdarahan • MRI: Kay dan Spritzer (1991) diskusikan aspek
pada jalan lahir setelah kehamilan 28 minggu. positif teknik ini.
Insiden : 2-5% seluruh persalinan • Placenta yang terletak dekat os interna tetapi
Klasifikasi perdarahan antepartum yaitu : tidak menutupi selama trimester kedua atau
1. plasenta previa (20% APB) awal trimester ketiga kecil untuk tetap tjd plac
2. Solusio plasenta (40% APB) previa.
3. Vasa previa / Insersio velamentosa • Penatalaksanaan plasenta previa
4.Ruptur sinus marginalis 1. Terapi Ekspektatif
5. Plasenta sirkumvalata - Rawat inap dan tirah baring
6. Tak terklasifikasi (35% APB) - Pemeriksaan USG
- Berikan tokolitik
Plasenta previa - Uji pematangan paru janin
merupakan plasenta yang letaknya abnormal 2. Terapi aktif
yaitu pada segmen bawah rahim, sehingga Untuk perdarahan yang aktif dan
menutupi sebagian atau seluruh pembukaan banyak
jalan lahir. 3. Seksio sesaria
Klasifikasi
1. Plasenta previa totalis 1. Janin preterm tetapi belum ada indikasi
2. Plasenta previa lateralis/parsialis untuk pelahiran.
3. Plasenta previa marginalis 2. Janin sudah matur.
4. Plasenta previa letak rendah 3. Sudah inpartu.
Etiologi 4. Perdarahan yang parah sehingga janin
Etiologi plasenta previa belum jelas harus dilahirkan walaupun masih
Faktor resiko terjadinya plasenta previa: imatur.
1. Merokok • Pelahiran: hampir semua kasus dg SC.
2. Pertambahan usia (>35 tahun) -Lakukan ligasi pembuluh darah bila
3. Riwayat seksio sesaria sebelumnya perlu (a. uterina atau a. iliaka interna.
4. Defek Vaskularisasi pada desidua
5. Plasenta yang besar dan luas HEPATITIS B
6.riwayat plasenta previa sebelumnya pada ibu hamil
7. multipara • Sembuh ( 90 %)
Diagnosis • Infeksi Akut-Hepatitis Fulminan
plasenta previa : • Pengidap kronik
- Adanya perdarahan pervaginam pada hamil * Pengidap sehat ( healthy carrier) :
28 minggu, tanpa sebab, berwarna merah - HBsAg (+), SGOT/SGPT Normal
segar dan tidak nyeri. - No Liver Defect
• Perdarahan tanpa nyeri - Transmisi (+) Vertical & Horizontal Trans.
• Perdarahan terutama terjadi pd saat inpartu. * Pengidap kronik (chronic hepatitis) - KHP/SH
• Perdarahan diperparah krn ketidakmampuan - HBsAg (+), SGPT/SGOT
miometrium di segmen bawah berkontraksi - Liver defect (+)
untuk menjempit pembuluh darah yang - Transmit HBV (+)
robek dibanding korpus uteri. - HBV-DNA integrasi dg sel hati KHP/ SH
• Diagnosis ditegakkan dg USG, pemeriksaan
klinis dg pemeriksaan serviks tidak dianjurkan hepatitis fulminan
• Terjadi sebesar 1% dari pengidap
Pemeriksaan Fisik • Mortalitas 70% (O Grady et al.,1988)
Pemeriksaan Luar : • Gejala:
- Bagian terbawah janin belum masuk PAP , *Sangat ikterik, nyeri perut ka. atas,
sering terdapat kelainan letak janin. uro.& bilirubin positif,ALT & AST tinggi
• Pemeriksaan Inspekulo diatas 1000, samnolensia dll.
Untuk mengetahui asal perdarahan *Bayi, tgt dari derajat kerusakan hepar
• Perabaan Fornices *Kemungkinan HPP sangat besar
Pemeriksaan ini bermakna bila janin letak TRANSMISI IBU KE JANIN
kepala. intrauteri, perinatal, post natal
• Pemeriksaan dalam : tidak dianjurkan
• Pemeriksaan anjuran : USG PREDISPOSISI FACTOR
• USG: transabdominal akurasi 96%, false positif • Titer DNA ( > 3,5 pg/ml)
tjd bila VU distensi. • HBeAg (+)
• USG transvaginal lebih baik dibanding • Infeksi VHB Akut pd trimester 3rd
transabdominal. USG transabdominal (75%,Tong,1981)
diperlukan konfirmasi dg USG transvaginal. • Vaccine escaped mutations :
Bayi dg HBsAg & Anti HBs positif (10 - 20%) The RBC indices has three parts:
• Partus lama ( lebih dari 16 jam ?) mean corpuscular volume (MCV),
which is the average red blood cell size
Ibu Bayi hari 0 Bayi 1 bl Bayi 6 bl
mean corpuscular hemoglobin (MCH),
Vaksinasi which is the amount of hemoglobin per
Titer DNA-VHB Plasenta red blood cell
PCR 0
<3,5 pg/ml (-) Infeksi - mean corpuscular hemoglobin
PCR (-) concentration (MCHC), which is the
³ 3,5 pg/ml
(+)
Infeksi
Intra Uterin
amount of hemoglobin relative to the
(PCR +,HBsAg - )
size of the cell or hemoglobin
Penularan
³ 12,5 – 22,5 pg/ml (+)
Infeksi vertikal +
concentration per red blood cell
Intra Uterin
(PCR +, HBsAg +)
According to the American Association for
³ 37,5 pg/ml
(+)
Clinical Chemistry, normal values for RBC indices
Infeksi +
are:
Persalinan
Bagan: Terjadinya Inf. VHB menurut titer virus ( Surya , 1997)
The MCV should be 80 to 96 femtoliters.
The MCH should be 27 to 33 picograms
H.B. Immunization by HBV Prevalence per cell.
The MCHC should be 33.4 to 35.5 grams
Endemicity per deciliter.
* Low : - Before exposure
High risk : medical, patient, drug adict., homosex. High MCV
- After exposure The MCV is higher than normal when red blood
babies born by HBsAg (+) mothers cells are larger than normal. This is called
macrocytic anemia.
HBV (+) couple
Macrocytic anemia can be caused by:
needle stick in juries
Vitamin B-12 deficiency
* Moderate / High : folate deficiency
- Before exposure : all babies chemotherapy
- After exposure : babies of HBsAg (+) mother preleukemias
1. Pasive Immunization HBIG Low MCV
2. Active Immunization The MCV will be lower than normal when red
- Plasm vaccine blood cells are too small. This condition is called
- Recombinant vaccine microcytic anemia.
- Containing vaccine Pre S2 (+Pre S1) Microcytic anemia may be caused by:
- Inprogess / developed : iron deficiency, which can be caused
- Recombinan Vaccine at Vaccinia virus by poor dietary intake of iron, menstrual
- Therapeutic Vaccine : bleeding, or gastrointestinal bleeding
TH + Epitop Sel TC (HBcAg 18 – 27) thalassemia
+ Ajuvan (Tetanus Toksoid) ) lead poisoning
3. Pasive - Active immunization chronic diseases
Normal MCV
Mother to Infant HBV transmission start by If you have a normal MCV, it means that your red
screening HBsAg to pregnant women than blood cells are normal in size. You can have a
followed by normal MCV and still be anemic if there are too
selective Immunization. few red blood cells or if other RBC indices are
HBV prevention mean , primary prevention to abnormal. This is called normocytic anemia.
HCC and Normocytic anemia occurs when the red blood
HC and increasing the quality of life of the next cells are normal in size and hemoglobin content,
generation. but there are too few of them. This can be
Universal precaution should be done intensively caused by:
especially
a sudden and significant blood loss
to whom with highly contact to blood.
Obsterician and pediatrician should be work a prosthetic heart valve
hand in hand in a tumor
the prevention of mother to infant HBV a chronic disease, such as a kidney
transmission. disorder or endocrine disorder
aplastic anemia
a blood infection
High MCHC
If you have a high MCHC, this means that the
relative hemoglobin concentration per red
blood cell is high. MCHC can be elevated in
diseases such as:
hereditary spherocytosis
sickle cell disease
homozygous hemoglobin C disease
Low MCHC
If you have a low MCHC, it means that the
relative hemoglobin concentration per red
blood cell is low. The red blood cells will take on
a lighter color when viewed under the
microscope. Individuals with anemia and a
corresponding low MCHC are said to be
hypochromic. Conditions that can cause low
MCHC include the same conditions that cause
low MCV, including:
iron deficiency
chronic diseases
thalassemia
lead poisoning
Generally, a low MCV and a MCHC will be found
together. Anemias in which both MCV and
MCHC are low are called microcytic,
hypochromic anemia
Anda mungkin juga menyukai
- BpjsDokumen76 halamanBpjsWelki Vernando75% (4)
- Raymond Dwi Prasetya - 42200429 - CRITICAL APPRAISALDokumen13 halamanRaymond Dwi Prasetya - 42200429 - CRITICAL APPRAISALFajar SutrisnaBelum ada peringkat
- Kasus FisiologiDokumen3 halamanKasus FisiologiFajar SutrisnaBelum ada peringkat
- Transale BV JurnalDokumen8 halamanTransale BV JurnalFajar SutrisnaBelum ada peringkat
- Aplikasi Klinis Corneal Collagen Cross Linking CXL - Tommy Tri AtmajaDokumen14 halamanAplikasi Klinis Corneal Collagen Cross Linking CXL - Tommy Tri AtmajaPrawira DarmaBelum ada peringkat
- Translate MataDokumen5 halamanTranslate MataFajar SutrisnaBelum ada peringkat
- MastoiditisDokumen7 halamanMastoiditisPrawira DarmaBelum ada peringkat
- LB, Tujuan, RM CLX-UlkusDokumen2 halamanLB, Tujuan, RM CLX-UlkusFajar SutrisnaBelum ada peringkat
- Penatalaksanaan UrtikariaDokumen32 halamanPenatalaksanaan UrtikariaAkhyar Sulaiman PattiradjaBelum ada peringkat
- Perda Cadangan Pangan OkeDokumen23 halamanPerda Cadangan Pangan OkeFajar SutrisnaBelum ada peringkat
- Uji Chi Square PDFDokumen10 halamanUji Chi Square PDFiin khoirinnisaBelum ada peringkat
- 23 28 Abdul RRDokumen6 halaman23 28 Abdul RRSuci NourmalizaBelum ada peringkat
- AbcdDokumen26 halamanAbcdbellaBelum ada peringkat
- Laporan Pendahuluan NSTEMIDokumen11 halamanLaporan Pendahuluan NSTEMIArik PratamaBelum ada peringkat
- Mengenal Pembagian SyokDokumen24 halamanMengenal Pembagian SyokFajar SutrisnaBelum ada peringkat
- 215 310 1 SMDokumen6 halaman215 310 1 SMHalimahBelum ada peringkat
- ATKDokumen10 halamanATKDarly PurbaBelum ada peringkat
- 10 Tips Menjaga Kesehatan MataDokumen4 halaman10 Tips Menjaga Kesehatan MataFajar SutrisnaBelum ada peringkat
- Uu No 44 2009 PDFDokumen40 halamanUu No 44 2009 PDFrahayuBelum ada peringkat
- 15 29 2 PB PDFDokumen7 halaman15 29 2 PB PDFVazia Rahma HandikaBelum ada peringkat
- Compartment Syndrome PDFDokumen13 halamanCompartment Syndrome PDFFajar SutrisnaBelum ada peringkat
- Diagram FisboneDokumen5 halamanDiagram FisbonefebiBelum ada peringkat
- Tutor 25 Mar 2019Dokumen8 halamanTutor 25 Mar 2019Fajar SutrisnaBelum ada peringkat
- Tutor 30 Agustus 2018Dokumen7 halamanTutor 30 Agustus 2018Fajar SutrisnaBelum ada peringkat
- TutorDokumen6 halamanTutorFajar SutrisnaBelum ada peringkat
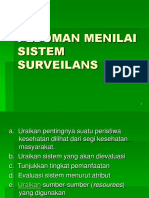
- 2 Pedoman Surveilan Dan ResponDokumen21 halaman2 Pedoman Surveilan Dan ResponJuleBelum ada peringkat
- Tutor 26 April 2018Dokumen12 halamanTutor 26 April 2018Fajar SutrisnaBelum ada peringkat
- Luka Bakar Referat Bedah PDFDokumen22 halamanLuka Bakar Referat Bedah PDFGafuran Lavazquez100% (1)
- EDUKASIDokumen1 halamanEDUKASIFajar SutrisnaBelum ada peringkat