s41577 020 00434 6.en - Id
Diunggah oleh
Deys AmirJudul Asli
Hak Cipta
Format Tersedia
Bagikan dokumen Ini
Apakah menurut Anda dokumen ini bermanfaat?
Apakah konten ini tidak pantas?
Laporkan Dokumen IniHak Cipta:
Format Tersedia
s41577 020 00434 6.en - Id
Diunggah oleh
Deys AmirHak Cipta:
Format Tersedia
Diterjemahkan dari bahasa Inggris ke bahasa Indonesia - www.onlinedoctranslator.
com
Ulasan
Pertimbangan imunologis untuk
strategi vaksin COVID-19
Mangalakumari Jeyanathan1,2,3,5, Sam Afkhami1,2,3,5, Fiona Smaill2,3,
Matthew S. Miller1,3,4, Brian D. Lichty1,2✉ dan Zhou Xing1,2,3✉
Abstrak | Pandemi penyakit coronavirus 2019 (COVID-19) yang disebabkan oleh
sindrom pernafasan akut parah coronavirus 2 (SARS-CoV-2) adalah tantangan paling
berat bagi umat manusia dalam satu abad. Dipercaya secara luas bahwa keadaan
normal sebelum pandemi tidak akan pernah kembali sampai strategi vaksin yang
aman dan efektif tersedia dan program vaksinasi global berhasil diterapkan. Di sini,
kami membahas prinsip-prinsip imunologi yang perlu dipertimbangkan dalam
pengembangan strategi vaksin COVID-19. Berdasarkan prinsip-prinsip ini, kami
memeriksa kandidat vaksin COVID-19 saat ini, kekuatan dan potensi kekurangan
mereka, dan membuat kesimpulan tentang peluang keberhasilan mereka. Akhirnya,
Wabah penyakit coronavirus 2019 (COVID-19) pertama kali merupakan strategi vaksin COVID-19 yang aman dan efektif
dilaporkan di Wuhan, Cina, pada akhir 2019 dan, pada saat artikel secara imunologis, bagaimana menentukan titik akhir yang
ini ditulis, telah menyebar ke 216 negara dan wilayah1. Itu telah berhasil dalam pengujian kemanjuran vaksin dan apa yang
membuat dunia terhenti. Patogen virus pernapasan parah diharapkan dari upaya vaksin global selama beberapa tahun
sindrom pernapasan akut coronavirus 2 (SARS-CoV-2) telah ke depan. Tinjauan ini menguraikan prinsip-prinsip
menginfeksi setidaknya 20,1 juta orang dan membunuh lebih imunologi panduan untuk desain strategi vaksin COVID-19
dari 737.000 orang di seluruh dunia, dan terus bertambah.1. dan menganalisis lanskap vaksin COVID-19 saat ini dan
Meskipun jarak fisik dan strategi mitigasi penularan lainnya yang tantangan ke depan.
diterapkan di sebagian besar negara selama pandemi saat ini
telah mencegah sebagian besar warganya terinfeksi, strategi ini Kekebalan alami dan yang diinduksi oleh vaksin
secara paradoks akan membuat mereka tidak memiliki kekebalan Meskipun masih banyak yang harus dipahami mengenai
1Imunologi McMaster
terhadap SARS-CoV-2 dan dengan demikian rentan terhadap respons imun terhadap SARS-CoV-2, dan imunitas
Pusat Penelitian, Universitas
gelombang infeksi tambahan. Pekerja perawatan kesehatan, protektif yang diinduksi vaksin mungkin berbeda dari
McMaster, Hamilton,
ON, Kanada. manula dan mereka yang memiliki kondisi kesehatan yang imunitas alami karena strategi penghindaran imun virus,
2Departemen Patologi dan
mendasari berada pada risiko yang sangat tinggi2–4. Sudah pemahaman yang lebih baik tentang respons imun alami
Kedokteran Molekuler, diterima secara luas bahwa dunia tidak akan kembali ke keadaan akan berperan dalam mengembangkan vaksin yang
Universitas McMaster, normal sebelum pandemi sampai vaksin yang aman dan efektif efektif dan strategi terapi. Sangat relevan untuk
Hamilton, ON, Kanada. tersedia dan program vaksinasi global berhasil dilaksanakan.5. memahami perbedaan respons imun antara kasus tanpa
3Michael G. DeGroote Institut gejala, ringan dan berat serta pada tahap awal dan akhir
Penelitian Penyakit Menular,
Karena COVID-19 baru bagi umat manusia dan sifat infeksi, dan untuk memahami mengapa manula sangat
Universitas McMaster,
Hamilton,
respons imun protektif kurang dipahami, tidak jelas strategi rentan terhadap COVID-19, sedangkan yang muda lebih
ON, Kanada. vaksin mana yang paling berhasil. Oleh karena itu, sangat terlindungi. Diperkirakan bahwa 40-75% infeksi mungkin
4Departemen Biokimia dan penting untuk mengembangkan berbagai platform dan ringan atau tanpa gejala7,8dan individu tanpa gejala
Ilmu Biomedis, Universitas strategi vaksin secara paralel. Memang, sejak wabah dimulai, mungkin memiliki durasi pelepasan virus yang jauh lebih
McMaster, para peneliti di seluruh dunia telah berlomba untuk lama daripada rekan-rekan mereka yang bergejala9.
Hamilton, ON, Kanada.
mengembangkan vaksin COVID-19, dengan setidaknya 166 Lebih lanjut, individu yang asimtomatik dan sakit ringan
5Penulis-penulis ini memberikan kontribusi
kandidat vaksin saat ini dalam pengembangan praklinis dan tampaknya mengembangkan kekebalan yang dimediasi
yang sama: Mangalakumari
klinis.5(Ara.1). Untuk memenuhi kebutuhan mendesak akan antibodi tingkat rendah memiliki implikasi penting untuk
Jeyanathan, Sam Afkhami.
vaksin, paradigma pengembangan vaksin pandemi baru memahami kekebalan kelompok.
✉surel:blichty@mac.com;
xingz@mcmaster.ca telah diusulkan yang mempersingkat waktu pengembangan Situs awal infeksi SARS-CoV-2 adalah saluran pernapasan
https://doi.org/10.1038/
dari 10-15 tahun menjadi 1-2 tahun.6. Namun, masih ada 10,11. Saat masuk, SARS-CoV-2 berinteraksi dengan reseptor
s41577-020-00434-6 ketidakjelasan tentang apa yang mungkin angiotensin-converting enzyme 2 (ACE2)
ULASAN ALAM|Imunologi volume 20 | oktober 2020 |615
Ulasan
yang dihasilkan dari penekanan kekebalan bawaan mungkin
7 mendukung respons inflamasi yang tidak teratur berikutnya
16,21, terutama pada kasus COVID-19 yang parah. Kasus-kasus
seperti itu ditandai dengan peningkatan jumlah monosit
inflamasi dan neutrofil dalam darah20,22,23dan CD14+CD16+
makrofag yang diturunkan monosit di saluran napas20,24, dan
38 peningkatan kadar sitokin dan kemokin inflamasi sistemik20,
50
22,23. Kegagalan untuk mencapai kontrol awal infeksi SARS-
protein CoV-2 di saluran pernapasan kemungkinan mengakibatkan
subunit rekombinan beban virus yang tinggi dan disregulasi, berpotensi
vektor virus mematikan, respons inflamasi dan imunopatologi, termasuk
sindrom kesulitan pernapasan akut. Untuk itu, se-
orang tua dan mereka yang memiliki penyakit penyerta mungkin
4 sangat rentan terhadap COVID-19 karenaimunosenesensidan
Seperti virus Nukleat kecenderungan mereka untuk meningkatkan respons inflamasi
3 partikel berbasis asam yang berlebihan25–27. Selain pertimbangan imunitas adaptif yang
1
Hidup diinduksi vaksin yang dibahas kemudian, dimasukkannya konsep
dilemahkan tidak aktif yang baru-baru ini muncul tentangkekebalan terlatih (Kotak1)
virus 12 virus
27 dalam desain vaksin COVID-19 dapat lebih meningkatkan
perlindungan, terutama pada fase awal infeksi.
5
9 10 Respon antibodi.Antibodi IgM dan IgG terhadap SARS-CoV-2
dapat dideteksi dalam 1-2 minggu setelah timbulnya gejala
pada sebagian besar individu yang terinfeksi.28. Meskipun
Perkembangan praklinis Perkembangan klinis hubungan antara antibodi penetralisir dan sel T spesifik
antigen dan keparahan penyakit dan hasil klinis masih harus
dipahami, tingkat antibodi penetralisir yang tinggi telah
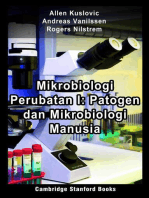
Gambar 1 |Lanskap vaksin COVID-19 global.Enam jenis utama kandidat vaksin untuk
penyakit coronavirus 2019 (COVID-19) diilustrasikan (virus hidup yang dilemahkan, vektor diamati pada individu yang pulih.29, yang berkorelasi dengan
virus rekombinan, virus yang tidak aktif, subunit protein, partikel mirip virus dan berbasis respons sel T, terutama respons CD4+sel T30, dan tampaknya
asam nukleat), menunjukkan jumlah kandidat vaksin yang sedang dalam pengembangan menawarkan beberapa manfaat dalam studi pengobatan
klinis dan praklinis. Platform berbasis asam nukleat mencakup vaksin mRNA (6 klinis dan dengan plasma konvalesen31. Studi terbaru menunjukkan
16 praklinis) dan vaksin DNA plasmid (4 klinis dan 11 praklinis). Data diperoleh dariref.5. bahwa besarnya respons antibodi penetralisir berkorelasi
positif dengan tingkat keparahan penyakit32. Jadi, sementara
respons antibodi berkurang dalam beberapa minggu setelah
pada sel epitel bronkus dan alveolus melalui domain infeksi pada kebanyakan orang yang terinfeksi SARS-CoV-2(
pengikat reseptor protein spike (S) (RBD), yang kemudian ref.32), yang merupakan ciri respons antibodi terhadap virus
dipancing oleh protease serin seluler spesifik, transmembran corona 'common cold' lainnya17, besarnya respon antibodi
protease serin 2 (TMPRSS2), untuk mendapatkan entri12,13. penetralisir pada individu tanpa gejala tidak hanya lebih kecil
Analisis transkrip yang mengkode ACE2 dan TMPRSS2 tetapi juga menurun lebih cepat dibandingkan pada individu
Sindrom kesulitan dengan sekuensing RNA sel tunggal telah menunjukkan yang bergejala.9.
pernapasan akut
bahwa transkrip ini diekspresikan bersama dalam berbagai Target utama antibodi penawar virus corona adalah
Suatu kondisi paru-paru yang
berkembang pesat yang ditandai jenis sel10,11, dan dari studi otopsi SARS-CoV-2 dapat dideteksi protein S, yang terdiri dari domain S1 dan S2. S1 adalah
dengan kekurangan pertukaran di beberapa organ, termasuk paru-paru, faring, jantung, membran distal dan berisi RBD yang mengikat reseptor
oksigen dan sesak napas, akibat hati, otak dan ginjal.14. seluler ACE2. S2 adalah proksimal membran dan
cedera paru-paru yang parah dan
memiliki peran dalam fusi membran33. Protein S dari
peradangan berikut
infeksi.
Respon imun bawaan.Bukti yang muncul menunjukkan SARS-CoV dan SARS-CoV-2 adalah 88% identik dan
bahwa respons imun terhadap SARS-CoV-2 serupa dalam keduanya mengikat ACE2 dengan afinitas tinggi33.
Imunosenesensi beberapa aspek dengan respons terhadap SARS-CoV atau Antibodi monoklonal dan poliklonal tertentu yang
Perubahan terkait usia dalam sistem
coronavirus sindrom pernapasan Timur Tengah (MERS-CoV), dinaikkan ke protein S SARS-CoV dapat menetralkan
kekebalan yang mengarah pada
dua virus corona yang bertanggung jawab atas wabah SARS silang SARS-CoV-2(referensi33,34). Antibodi yang berikatan
penurunan progresif dalam
kemampuannya untuk mengembangkan
2002-2004 dan Wabah MERS 2012 yang masing-masing dengan S1 RBD memblokir interaksinya dengan ACE2,
antibodi dan seluler yang efektif berasal dari China dan Arab Saudi15–17. Seperti SARS-CoV dan sedangkan antibodi yang mengikat ke wilayah lain S1
respon terhadap infeksi MERS-CoV, SARS-CoV-2 menekan aktivasi sistem kekebalan dan S2 dapat menghambat perubahan konformasi
dan vaksinasi.
bawaan, termasuk sel dendritik18,19, dan meredam respons protein S dan memblokir fusi membran.35–37.
Kekebalan terlatih
interferon antivirus tipe I dan tipe III20. Kemampuan SARS- Selama respons imun alami terhadap SARS-CoV-2, titer
Keadaan reset yang menetap dari CoV-2 untuk menumbangkan respons imun bawaan ini antibodi yang tinggi juga dihasilkan terhadap nukleoprotein
sistem imun bawaan lama setelah dapat menjelaskan masa inkubasi yang berkepanjangan (N) — protein virus yang paling melimpah.38–40. Meskipun
antigen awal atau paparan mikroba
atau periode presimptomatik 2-12 hari untuk COVID-19 antibodi terhadap N tidak mungkin menetralisir virus,
yang mengarah pada peningkatan
dibandingkan dengan masa inkubasi 1-4 hari untuk mereka telah dilaporkan memberikan perlindungan
respons terhadap antigen atau
mikroorganisme yang sama atau influenza.16. Dengan demikian, replikasi SARS-CoV-2 yang terhadap virus hepatitis tikus, virus corona tikus. Khususnya,
tidak terkait. tidak terkontrol pada fase awal infeksi antibodi ini adalah IgG2a, menunjukkan
616|oktober 2020 | volume 20 www.nature.com/nri
Ulasan
CD8 . sitotoksik tidak lengkap+Sel T sangat penting untuk
Kotak 1 |Kekebalan yang terlatih sebagai strategi vaksin COVID-19 yang potensial
pembersihan virus49. Satu penelitian menemukan bahwa di
Memori kekebalan bawaan (juga dikenal sebagai kekebalan terlatih) adalah komponen antara orang yang telah pulih dari COVID-19, 100% memiliki CD4
memori imunologis yang baru-baru ini dikenal yang memiliki implikasi untuk strategi vaksin83, spesifik protein S+Sel T dalam sirkulasi dan 70% memiliki CD8 .
84,168,169 . Beberapa vaksin manusia hidup yang dilemahkan menginduksi kekebalan terlatih
spesifik protein S+sel T dalam sirkulasi30, dan studi praklinis
yang dapat memediasi respons protektif non-spesifik terhadap infeksi heterolog selain
menunjukkan peran protektif sel T dalam pertahanan inang
memori imun adaptif patogenspesifik.168–170. vaksin manusia yang paling banyak dipelajari
terhadap SARS-CoV50.
yang menginduksi kekebalan terlatih adalah vaksin bacillus calmette-Guérin (bcG) melawan
tuberkulosis171. Vaksinasi bcG memberi monosit yang bersirkulasi dengan karakteristik Masa inkubasi 2-12 hari atau periode presimptomatik
kekebalan terlatih melalui pemasangan ulang epigenetik dan metabolik dari nenek moyang infeksi SARS-CoV-2 dikaitkan tidak hanya dengan penekanan
myeloid di sumsum tulang169,172,173. monosit terlatih ini meningkatkan perlindungan terhadap kekebalan bawaan yang dimediasi virus tetapi juga dengan
infeksi heterolog, termasuk infeksi virus pernapasan174–176. Oleh karena itu bcG dapat aktivasi sel T yang tertunda, terutama CD8.+sel T18,19, seperti
menawarkan tingkat perlindungan dari penyakit coronavirus 2019 (covID-19), yang mungkin halnya SARS dan MERS. Orang yang telah pulih dari
didukung oleh korelasi terbalik yang diamati antara vaksinasi bcG universal dan kematian COVID-19 tampaknya memiliki tingkat antibodi penetralisir
akibat covid-19.177. Beberapa uji klinis sedang dilakukan untuk menilai efek bcG atau vaksinasi dan sel T yang tinggi, dan, dibandingkan dengan kasus yang
campak pada covid-19 (ref.178).
parah, kasus COVID-19 yang lebih ringan memiliki jumlah
Vaksin covid-19 yang dapat menginduksi kekebalan terlatih dapat meningkatkan
CD8 memori yang lebih besar.+Sel T di saluran pernapasan24,
pengendalian virus dini dengan mengatasi penekanan kekebalan bawaan yang disebabkan
29,30. Bukti menunjukkan bahwa induksi sel T memori residen
oleh virus dan memfasilitasi aktivasi kekebalan adaptif. waktu awal tindakan oleh kekebalan
terlatih adalah penting karena kelebihan produksi sitokin oleh makrofag pada tahap jaringan paru (TRMsel) akan tergantung pada rute vaksinasi.
selanjutnya dari covid-19 dapat berkontribusi pada imunopatologi. Meskipun masih harus vaksinasi mukosa pernafasanmenginduksi T . paru yang kuatRM
dipahami bagaimana cara terbaik memanfaatkan kekebalan terlatih untuk strategi vaksin respon sel, sedangkanvaksinasi parenteralgagal melakukannya
covid-19, bukti terbaru menunjukkan bahwa rute paparan mikroba atau vaksinasi 51–53. Secara eksperimental, T jalan napasRMsel yang
menentukan distribusi jaringan kekebalan terlatih.83,84,169. Karena kekebalan mukosa ditimbulkan oleh vaksinasi mukosa pernapasan menawarkan
pernapasan adalah kunci untuk pembersihan awal sindrom pernapasan akut parah perlindungan yang kuat terhadap infeksi SARS-CoV54.
coronavirus 2 (SARS-cov-2), menginduksi kekebalan terlatih dalam makrofag alveolar dan sel
bawaan lainnya83,179–181melalui vaksinasi mukosa pernafasan bisa menjadi strategi yang
Sel T helper (THsel) fenotipe sel T yang diinduksi vaksin
efektif. Memang, vaksin vektor adenovirus serotipe 5 manusia yang dikirim ke mukosa
juga relevan dengan perlindungan yang dimediasinya. Kasus
pernapasan menginduksi makrofag alveolar memori yang mampu melatih kekebalan
SARS yang tidak terlalu parah dikaitkan dengan percepatan
terhadap infeksi heterolog.85. Namun, tidak jelas apakah makrofag memori paru dapat
digantikan oleh monosit inflamasi sebagai respons terhadap SArS-cov-2. induksi T .Hrespon 1 sel55, sedangkan TH2 tanggapan sel telah
dikaitkan dengan peningkatan penyakit paru-paru setelah
infeksi pada inang yang divaksinasi secara parenteral
bahwa mereka dapat memberikan perlindungan melalui dengan vaksin virus SARS-CoV yang tidak aktif56,57. Dengan
Fungsi efektor yang dimediasi Fcdaripada netralisasi virus secara demikian, T . yang diinduksi oleh vaksin COVID-19RMsel harus
langsung41,42. Agak tidak biasa, beberapa penelitian telah memiliki TH1 fenotipe mirip sel.
melaporkan bahwa respons IgA terhadap protein S Garis-garis bukti ini, bersama dengan data yang
memuncak lebih awal daripada respons IgM dan lebih jelas, menunjukkan bahwa imunitas yang diperantarai sel T umumnya
yang menjadikan IgA target yang berpotensi menarik untuk merupakan korelasi perlindungan vaksin yang lebih andal
tes diagnostik berbasis antibodi.43,44. Dasar mekanistik dari daripada titer antibodi pada manula.26, sangat mendukung
induksi awal IgA spesifik-S ini belum jelas. dimasukkannya respons sel T dalam desain vaksin COVID-1917,27.
Kami belum memahami daya tahan respons antibodi
Efektor yang diperantarai Fc terhadap SARS-CoV-2. Namun, penelitian longitudinal Kekebalan reaktif silang yang sudah ada sebelumnya.
fungsi sebelumnya pada pasien dengan infeksi SARS-CoV melaporkan Bukti yang muncul menunjukkan bahwa CD4+Sel T pada 35%
fungsi kekebalan yang
penurunan substansial dari titer antibodi penetralisir antara 1 orang sehat yang tidak terpajan SARS-CoV-2 mengenali
dimediasi melalui interaksi
regio Fc konstan dari tahun dan 2 tahun setelah infeksi.45,46. Ini konsisten dengan protein SARS-CoV-2 S dan CD4 itu+Sel T pada 40-60% individu
antibodi dengan molekul penelitian klasik yang menunjukkan penurunan antibodi yang yang tidak terpapar reaktif terhadap protein SARS-CoV-2
imun bawaan, protein relatif cepat terhadap virus corona musiman 229E47. Saat ini tidak selain protein S30,58. Hal ini menunjukkan adanya reaktivitas
pelengkap dan reseptor Fc
ada korelasi kekebalan perlindungan untuk SARS-CoV-2 atau virus silang antara CD4+Sel T spesifik untuk SARS-CoV-2 dan CD4+
khusus yang diekspresikan
oleh sel imun bawaan.
korona manusia lainnya. Dengan demikian, tidak jelas titer Sel T khusus untuk virus corona flu biasa, SARS-CoV, dan
Fungsi yang dihasilkan antibodi penetralisir apa yang cukup untuk memberikan betacoronavirus hewan17,59–61. Ada empat virus corona pada
meliputi komplemen- perlindungan terhadap infeksi. Membangun korelasi semacam manusia — 229E, NL63, OC43, dan HKU1 — yang
sitotoksisitas tergantung dan fagositosis
itu akan sangat penting untuk memandu pengembangan vaksin menyebabkan ~ 15% flu biasa pada manusia17. Orang
seluler yang bergantung pada antibodi
COVID-19 yang efektif. dewasa dapat terinfeksi dengan salah satu dari ini rata-rata
atau sitotoksisitas yang dimediasi sel.
setiap 2-3 tahun, sehingga mungkin ada tingkat kekebalan
imunitas yang diperantarai sel T.Sementara vaksin reaktif silang yang sudah ada sebelumnya terhadap antigen
mukosa pernafasan antivirus manusia yang berhasil saat ini, seperti vaksin SARS-CoV-2 pada orang-orang ini, yang menawarkan
vaksinasi
influenza dan campak, sebagian besar bergantung pada penjelasan potensial untuk kerentanan yang berbeda
Pemberian langsung vaksin ke
saluran pernapasan baik dengan
induksi respons antibodi, bukti yang muncul menunjukkan terhadap SARS. - Infeksi CoV-2 Selain memahami hubungan
pemberian intranasal atau persyaratan imunitas yang dimediasi antibodi dan sel T antara kekebalan yang sudah ada sebelumnya terhadap
inhalasi aerosol. untuk perlindungan yang efektif terhadap SARS-CoV-2.( virus corona manusia dan pertahanan inang terhadap SARS-
referensi17,27). Diketahui bahwa CD4+Bantuan sel T penting CoV-2, penting juga untuk mempertimbangkan kontribusi
Vaksinasi parenteral
untuk respons antibodi yang optimal dan untuk CD8+Aktivasi respons imun lintas-reaktif yang didorong oleh vaksin
Pemberian vaksin melalui
kulit, otot atau pembuluh sel T dalam pertahanan inang48. Selanjutnya, jika penetralan COVID-19 terhadap kekebalan protektif yang diinduksi
darah. perlindungan yang dimediasi antibodi vaksin. .
ULASAN ALAM|Imunologi volume 20 | oktober 2020 |617
Ulasan
Yang penting, sedangkan CD4+Sel T dari pasien COVID-19 peningkatan yang bergantung pada antibodi(ADE) penyakit. ADE
Tergantung antibodi
peningkatan sama-sama mengenali subunit S1 dan S2 dari SARS-CoV-2, paling klasik terkait dengan virus dengue, di mana
(Ade). ADe penyakit terjadi CD4 cross-reaktif+Sel T dari individu yang tidak terpajan konsentrasi antibodi yang reaktif-silang tetapi subnetralisasi
saat diinduksi vaksin mengenali subunit S258. CD4+Sel T dari pasien dengan terhadap satu serotipe virus meningkatkan infeksi dengan
antibodi yang tidak menetralkan atau
COVID-19 bereaksi silang kuat dengan subunit S2 dari serotipe lain dalam sel pembawa reseptor Fcγ (FcγR),
menetralkan dengan lemah mengikat
virus yang baru menginfeksi untuk
coronavirus manusia OC43 dan 229E. Lebih dari 90% orang termasuk makrofag62. Sifat umum di antara virus yang
mempromosikan virus yang ditingkatkan dewasa sehat yang diuji juga memiliki antibodi IgG khusus menyebabkan ADE adalah kemampuan untuk bereplikasi
penyerapan ke dalam sel inang untuk keempat virus corona flu biasa manusia17. Namun, dalam makrofag dan/atau menyebabkan mereka merespons
melalui reseptor Fcγ.
mirip dengan respons antibodi terhadap SARS-CoV dan secara tidak normal. Meskipun makrofag tampaknya tidak
Fenomena ini telah diamati
SARS-CoV-2, respons antibodi terhadap virus corona menjadi target utama infeksi SARS-CoV-2, dan ekspresi ACE2
eksperimental atau klinis setelah
vaksinasi terhadap patogen virus manusia berkurang dengan cepat dalam beberapa bulan pada populasi monosit dan makrofag yang berbeda sangat
seperti virus dengue, virus setelah infeksi. Oleh karena itu, pengendalian reinfeksi bervariasi, data sebelumnya mengenai SARS-CoV
pernapasan syncytial dan virus dengan coronavirus manusia tampaknya terutama tidak menunjukkan bahwa FcγRs dapat memfasilitasi penyerapan
corona kucing.
bergantung pada antibodi tetapi bergantung pada sel T17. virus ke dalam makrofag. dan sel B21,63. Profil sitokin dari
Aktivasi makrofag Karena sel T reaktif silang coronavirus dapat spesifik pasien yang terinfeksi SARS-CoV-2 menyerupai
sindroma untuk protein virus struktural dan non-struktural58,61, tingkat mereka disindrom aktivasi makrofagdan bersifat
Juga dikenal sebagai badai respons sel T reaktif silang yang didorong oleh vaksin yang dipicu oleh sitokin dan kemokin inflamasi tingkat tinggi21,64–66
sitokin atau limfositosis
diinduksi oleh sebagian besar subunit protein dan vaksin . Selanjutnya, pasien dengan gejala COVID-19 dilaporkan
hemofagositosis sekunder.
COVID-19 vektor virus rekombinan, yang saat ini hanya menghasilkan antibodi IgG dengan tingkat fukosilasi yang
Keadaan klinis
hiperinflamasi sistemik yang didasarkan pada protein S, akan berbeda dari yang didorong berkurang, yang pada gilirannya meningkatkan interaksi
dicirikan oleh oleh vaksin COVID-19 multivalen seperti yang didasarkan mereka dengan pengaktifan FcγRIIIa.67.
hipersitokinemia, pada virus SARS-CoV-2 yang tidak aktif. Satu pengecualian Bukti untuk ADE dalam konteks infeksi SARS-CoV tidak
demam, adenopati,
adalah penggunaan vaksin SARS-CoV-2 hidup yang langsung. Korelasi antara titer antibodi dan tingkat
hepatosplenomegali,
sitopenia dan aktivasi dilemahkan karena kekebalan reaktif silang yang sudah ada keparahan infeksi telah dilaporkan, tetapi tidak jelas apakah
koagulasi intravaskular. sebelumnya dapat membatasi potensi vaksin tersebut. titer antibodi yang tinggi berkontribusi terhadap penyakit
Akhirnya, perlu dicatat bahwa keberadaan kekebalan reaktif atau apakah infeksi berat menyebabkan titer antibodi yang
silang yang signifikan pada beberapa individu memerlukan lebih tinggi.68. Juga, makrofag yang dirawat in vitro dengan
pertimbangan stratifikasi peserta uji klinis yang menerima serum dari pasien dengan SARS memiliki profil sitokin
kandidat vaksin COVID-19 sesuai dengan status kekebalan inflamasi yang berlebihan69,70.
virus corona yang sudah ada sebelumnya. ADE telah dilaporkan pada beberapa model hewan praklinis
yang divaksinasi dengan vaksin SARS-CoV eksperimental. Ferrets
Peningkatan penyakit yang bergantung pada antibodi. yang divaksinasi dengan virus vaccinia yang dimodifikasi Vaksin
Hambatan potensial untuk pengembangan vaksin COVID-19 Ankara (MVA) yang mengekspresikan protein S full-length telah
yang aman dan manjur(Kotak2)adalah risiko bahwa titer meningkatkan infeksi dan hepatitis setelah tantangan71,72.
antibodi penetralisir yang tidak mencukupi dapat memicu Antibodi terhadap protein S dilaporkan menginduksi cedera paru
akut pada kera yang terinfeksi secara eksperimental berdasarkan
pemeriksaan histologis69. Sebaliknya, hamster yang divaksinasi
Kotak 2 |Pertimbangan keamanan untuk vaksin COVID-19
dengan protein SARS-CoV S rekombinan utuh terlindungi dari
Karena sebagian besar individu yang terinfeksi dengan sindrom pernafasan akut parah coronavirus infeksi meskipun antibodi memiliki kemampuan untuk
2 (SARS-cov-2) tidak menunjukkan gejala atau hanya mengembangkan gejala ringan dan vaksin memediasi masuknya SARS-CoV ke dalam sel B melalui FcγRII.(ref.
penyakit coronavirus 2019 (covID-19) sedang dikembangkan untuk mencapai tujuan akhir imunisasi
73).
massal global, keamanan vaksin sangat penting. sangat penting. Indikasi kurangnya pertimbangan
Apakah ADE terjadi dalam konteks infeksi SARS-CoV-2
keamanan juga dapat memicu gerakan antivaksinasi dan keraguan vaksin, yang akan
masih belum jelas tetapi memerlukan penyelidikan lebih
membahayakan efek yang diinginkan untuk mencapai kekebalan kelompok. Dalam hal ini, sebagian
besar uji klinis vaksin Covid-19 saat ini pada awalnya dilakukan pada orang dewasa sehat berusia 55
lanjut, dengan fokus langsung pada apakah antibodi
tahun atau lebih muda, dengan hanya beberapa uji coba tahap selanjutnya termasuk manula.98,99,115, meningkatkan keparahan penyakit dan, jika demikian,
146–148. populasi lansia yang sangat rentan dan mereka yang memiliki kondisi medis yang mencirikan sifat spesifik antibodi ini. Apa yang tampak
mendasarinya sangat membutuhkan vaksin yang sangat aman dan efektif. Sebagian besar masih jelas adalah bahwa tingkat antibodi penetralisir yang
belum jelas apakah vaksin covid-19 yang diuji coba pada awalnya akan aman untuk anak-anak dan tinggi dapat memediasi perlindungan. Menentukan titer
manula baik dalam jangka pendek maupun jangka panjang. Masih mungkin bahwa strategi vaksin antibodi penetralisir yang bersifat protektif, memastikan
yang berbeda dengan profil keamanan dan kemanjuran yang terbukti mungkin diperlukan untuk bahwa vaksin COVID-19 dapat mencapai titer ini dan
perlindungan pada manula.
menghindari penurunan antibodi ke tingkat
keamanan vaksin umumnya ditentukan oleh sifat platform vaksin, pilihan bahan pembantu,
subnetralisasi melalui peningkatan yang sering akan
cara dan rute pemberian vaksin, usia vaksin dan status kekebalan vaksin yang sudah ada
penting untuk meminimalkan kemungkinan ADE. Vaksin
sebelumnya.78. Misalnya, mereplikasi virus hidup yang dilemahkan atau vaksin vektor virus
mungkin tidak aman untuk rute vaksinasi mukosa pernapasan. Tidak juga bahan pembantu COVID-19 yang dirancang secara rasional yang
kekebalan tertentu seperti tawas dan protein yang diturunkan dari bakteri. Ketika strategi menghilangkan epitop yang menginduksi ADE, tidak
imunisasi prime-boost diperlukan, efek samping umumnya lebih sering dan intens setelah menetralisir, atau menetralkan dengan lemah demi yang
vaksinasi booster115. strategi vaksin untuk covid-19, seperti untuk beberapa infeksi virus diketahui memediasi respons protektif juga dapat
pernapasan lainnya, memerlukan pertimbangan keamanan tambahan terkait dengan meminimalkan kemungkinan peningkatan penyakit.
kemungkinan peningkatan penyakit yang bergantung pada antibodi dan peran kelebihan Akhirnya,74. Oleh karena itu, strategi vaksin yang
produksi dirancang untuk menginduksi antibodi penetralisir dan
sitokin proinflamasi pada imunopatologi paru. yang terakhir terutama berkaitan
kekebalan yang dimediasi sel T yang kuat dapat
dengan penerapan strategi vaksin mukosa pernapasan.
membantu mengurangi risiko ADE.
618|oktober 2020 | volume 20 www.nature.com/nri
Ulasan
Desain vaksin Biasanya, platform vaksin non-viral ini memerlukan beberapa
Desain vaksin menyangkut pemilihan antigen, platform vaksinasi untuk menginduksi kekebalan protektif, sedangkan
vaksin, dan rute serta rejimen vaksinasi. Pilihan platform vaksin berbasis virus hidup memiliki kemampuan untuk
vaksin menentukan kekuatan imunogenik relatif dari memberikan kekebalan 'satu suntikan'. Sama halnya dengan
antigen virus yang diturunkan dari vaksin, apakah platform non-viral, vaksin virus yang telah dimatikan terkadang
adjuvant imun diperlukan dan sifat imunitas protektif. memerlukan dimasukkannya adjuvant dan pemberian berulang
Atribut ini juga menentukan kesesuaian vaksin untuk untuk kemanjuran penuh.78. Ada pro dan kontra imunologi untuk
rute vaksinasi tertentu, dan apakah rejimen vaksinasi masing-masing teknologi ini seperti yang dibahas
prime-boost diperlukan untuk meningkatkan kekebalan nanti(Meja1).
protektif yang dimediasi vaksin dan daya tahannya.
Selanjutnya, pemilihan vaksin virus hidup yang Rute dan rejimen vaksinasi.Selain pemilihan antigen dan
dilemahkan atau rute vaksinasi mukosa pernapasan platform vaksin yang cermat, rute vaksinasi merupakan
akan memerlukan pengujian keamanan yang lebih ketat. pertimbangan integral dari strategi vaksin52,79. Hal ini sangat
(Kotak2). penting untuk patogen mukosa seperti SARS-CoV-2 dan
patogen yang perlindungan optimalnya tidak hanya
Pemilihan antigen SARS-CoV-2.Protein struktural yang membutuhkan antibodi penetral tetapi juga imunitas seluler
ada dalam virion infeksius meliputi protein S, protein N, bawaan dan adaptif.17,80. Jendela peluang terbaik untuk
protein matriks (M) dan protein amplop (E). Protein N pengendalian dan pembersihan SARS-CoV-2 adalah periode
melapisi genom RNA untai positif besar, yang asimtomatik atau presimptomatik COVID-19 (2-12 hari), yang
terbungkus dalam amplop lipid yang berasal dari kemungkinan memerlukan semua elemen pelindung
membran sel inang, di mana tiga protein lainnya (S, M kekebalan untuk ada di dalam mukosa pernapasan sebelum
dan E) dimasukkan. Dalam kasus SARS-CoV, telah entri virus16,17,27. Rute vaksinasi memiliki peran penting
ditunjukkan bahwa hanya antibodi yang diarahkan ke dalam menentukan hal ini52,81. Antibodi IgG protektif yang
protein S yang dapat menetralkan virus dan mencegah diinduksi oleh vaksinasi parenteral segera muncul di mukosa
infeksi75. Akibatnya, semua vaksin SARS-CoV-2 yang pernapasan, ini menjadi mekanisme utama di mana injeksi
sedang dikembangkan mengandung setidaknya intramuskular vaksin campak atau influenza menawarkan
sebagian dari protein S. Ini mungkin dibatasi hanya perlindungan pada manusia. Namun, rute vaksinasi ini tidak
untuk domain S1 atau RBD. dapat secara efektif menginduksi antibodi IgA mukosa atau
Antibodi yang tidak menetralkan protein S dan protein T .RMsel di paru-paru52,81. Sebagai perbandingan, rute
lain yang terpapar (E dan M) dihasilkan. Karena ada dugaan vaksinasi mukosa pernapasan mahir dalam menginduksi
peran antibodi non-penetralisir ini, serta antibodi penawar antibodi dan TRMsel-sel di mukosa pernapasan, serta
lemah, pada ADE penyakit, penyertaan protein struktural (N) kekebalan terlatih yang dimediasi makrofag52,54,80–85(Kotak1).
dan/atau non-struktural lainnya sebagai antigen vaksin Vaksin virus, subunit protein dan asam nukleat yang tidak
Partikel mirip virus dapat membantu menciptakan protein yang lebih seimbang. aktif tidak dapat diberikan melalui rute mukosa pernapasan
(VlP). Jenis vaksin subunit respon yang melibatkan imunitas humoral dan sel T. Ini bisa karena persyaratannya untuk bahan pembantu imun yang
berdasarkan beberapa protein berupa protein yang sangat diekspresikan seperti protein N berpotensi tidak aman dan pemberian berulang(Meja1).
turunan virus yang dirakit
atau protein fungsional yang sangat terkonservasi yang Sebaliknya, vaksin vektor virus rekombinan, terutama yang
untuk meniru organisasi dan
konformasi virus asli asli tetapi
memiliki peran penting dalam siklus hidup virus. Misalnya, menggunakan adenovirus serotipe 5 manusia (Ad5) atau
tidak memiliki genom virus. penyertaan enzim virus seperti RNA-dependent RNA adenovirus yang diturunkan dari simpanse (ChAd), aman dan
polymerase dalam desain vaksin dapat memastikan bahwa sangat efektif untuk vaksinasi mukosa pernapasan.79.
ia menargetkan semua strain varian yang muncul, karena
Ajuvan
protein ini sangat terkonservasi.59,76,77, bahkan di seluruh
Komponen biokimia
tambahan untuk antigen vaksin yang virus corona yang berasal dari kelelawar yang dapat muncul Seringkali, vaksin imunogenik lemah berdasarkan virus yang
disertakan dalam formulasi vaksin untuk sebagai ancaman bagi manusia di masa depan. tidak aktif, subunit protein, asam nukleat atau vektor virus seperti
membantu merangsang respons imun Ad26 memerlukan rejimen vaksinasi homolog berulang agar
adaptif terhadap antigen vaksin dengan
efektif. Memang, sebagian besar vaksin manusia saat ini
cara:
mengaktifkan sel imun bawaan.
Platform vaksin.Secara umum, platform vaksin dibagi menjadi membutuhkan dosis berulang. Karena belum diketahui strategi
seringkali, vaksin tidak hidup seperti enam kategori: virus hidup yang dilemahkan, vaksin vektor virus vaksin COVID-19 mana yang akan digunakan atau untuk berapa
virus yang tidak aktif, subunit rekombinan yang direkayasa untuk mengekspresikan antigen lama perlindungan yang diinduksi vaksin dapat bertahan pada
protein dan asam nukleat
patogen target secara in vivo, virus yang dinonaktifkan atau manusia, masih ada kemungkinan bahwa
vaksin membutuhkan
dibunuh, vaksin subunit protein,partikel mirip virus vaksinasi prime-boost homolog atau heterologreg-
adjuvant imun.
(VLP) dan vaksin berbasis asam nukleat (DNA atau mRNA). Secara imen akan diminta untuk mempertahankan perlindungan,
Homolog atau umum, vaksin memerlukan dua komponen: antigen dari patogen bahkan dengan platform mandiri yang kuat seperti ChAd. Rute
vaksinasi prime-boost target yang diberikan atau dihasilkan oleh penerima vaksin; dan yang sama atau berbeda dapat digunakan untuk pengiriman
heterolog
sinyal infeksi (seperti pola molekuler terkait patogen atau pola vaksin berulang.
Regimen imunisasi berulang yang
dirancang untuk meningkatkan dan
molekul terkait kerusakan) yang memperingatkan dan
mempertahankan respons imun yang mengaktifkan sistem kekebalan inang. Vaksin hidup yang Kandidat utama vaksin COVID-19
diinduksi vaksin. itu mungkin melibatkan dilemahkan secara alami dapat menyediakan kedua komponen Per 31 Juli 2020, terdapat 27 kandidat vaksin
pengiriman berulang dari vaksin yang
ini, sedangkan platform vaksin non-viral dapat menyediakan COVID-19 dalam evaluasi klinis dan 139 vaksin dalam
sama (homolog) atau pengiriman
antigen tetapi seringkali memerlukan penyediaan sinyal buatan pengembangan praklinis5(Ara.1). Dari 27 vaksin yang
berurutan dari
platform vaksin yang untuk memperingatkan sistem kekebalan yang dikenal sebagai menjalani evaluasi klinis(Meja2), tiga kandidat utama
berbeda (heterolog). bahan pembantu. adalah vektor-virus dan berbasis mRNA
ULASAN ALAM|Imunologi volume 20 | oktober 2020 |619
Ulasan
Tabel 1 |Immunological properties of major COVID-19 candidate vaccine platforms
Vaccine SARS-CoV-2 Neutralizing T cell response Pre-existing Route of Overall Other
platform antigens antibody antivector vaccination immunogenicity attributes
CD4+ CD8+ Lung
response immunity
TH cells T cells TRM cells
Viral-vectored vaccines
Ad5 (non- S protein Quality and TH1 cell Potent Induced High, age- Parenteral Strong with Ample human
replicating) durability response; by RM but dependent, (IM) in single delivery safety data; RM
affected by negative not IM prevalence clinical but hindered delivery helps
pre-existing effects from route in blood; low trials by pre-existing bypass antivector
antivector pre-existing prevalence antivector immunity; can
immunity antivector in respiratory immunity be delivered by
immunity tract inhaled aerosol
Ad26 (non- S protein Quality and TH1 cell Moderate Induced Medium Parenteral Weak; requires Established
replicating) durability response; by RM but prevalence (IM) in repeated or human safety
affected by negative not IM planned heterologous fromHIV and
pre-existing effects from route clinical boost Ebola vaccine
antivector pre-existing trials vaccination trials; RMdelivery
immunity antivector helps bypass
immunity antivector
immunity
ChAd (non- S protein Unimpeded TH1 cell Potent Induced Very low Parenteral Strong with Well-established
replicating) owing to response by RM but prevalence (IM) in single delivery human safety
lack of not IM clinical data; amenable
pre-existing route trials to RM delivery;
antivector can be used as
immunity a stand-alone
vaccine or in
prime–boost
regimens
VSV S protein Unimpeded TH1 cell Response Not None Parenteral Good with Successfully
(replicating) owing to not as induced (IM) in single delivery licensed
lack of strong as by IM previous platform for
pre-existing for Ad5 or route successful Ebola; not
antivector ChAd when Ebola known whether
immunity used as a vaccine it protects
stand-alone trials against RM viral
vaccine; pathogens
strong T cell
booster
Measles S protein? Quality and TH1 cell Good Not High Parenteral Weak relative Not extensively
and durability response induced prevalence or RM to adenovirus tested in humans;
influenza depend on when by owing to vectors potential
viruses whether delivered parenteral vaccination recombination of
(replicating) there is via RM route and natural live attenuated
pre-existing route infection influenza vectors
antivector in the lung
immunity and delivered via RM
vaccination route
route
Other vaccines
mRNA- S protein Unimpeded TH1 cell Depends Not None Parenteral Requires Adjuvant
based or RBD owing to or TH2 cell on choice induced (IM) in repeated required; unclear
vaccine encapsulated lack of depending of adjuvant by clinical delivery whether it is
in lipid pre-existing on adjuvant and parenteral trials amenable to RM
nanoparticle antivector formulation route vaccination
immunity
DNA- S protein Unimpeded TH1 cell Response Not None Parenteral Weaker than Adjuvant
based owing to not as induced (IM) in mRNA-based required; not
vaccine lack of strong as clinical vaccine; requires amenable to RM
pre-existing for some trials repeated vaccination
antivector of the viral delivery
immunity vectors
Live Multiple viral Strong TH1 cell Strong Induced No cross- Parenteral Requires only a Extensive safety
attenuated antigens induction response by RM but reactive (SC) single delivery testing required
virus not IM antibodies; for potential
route cross-reactive recombination
T cells from with wild-type
seasonal virus
coronavirus
infections
620 | october 2020 | volume 20 www.nature.com/nri
R e v i ews
Table 1 (cont.) | Immunological properties of major COVID-19 candidate vaccine platforms
Vaccine SARS-CoV-2 Neutralizing T cell response Pre-existing Route of Overall Other
platform antigens antibody antivector vaccination immunogenicity attributes
CD4+ CD8+ Lung
response immunity
TH cells T cells TRM cells
Other vaccines (cont.)
Inactivated Multiple viral Strong TH1 cell or Weak Not None Parenteral Weak; requires Adjuvant
virus antigens induction TH2 cell response induced (IM) repeated required;
depending vaccination alum often
on adjuvant used, which
enhances TH2
cell responses
possibly involved
in ADE
Protein S protein or Strong TH1 cell or Weak Not None Parenteral Weak; requires Adjuvant
subunit RBD induction TH2 cell response induced (IM) in repeated required; mostly
vaccine depending clinical vaccination unsuitable for
on adjuvant trials RM vaccination
Virus-like Multiple viral Strong TH1 cell or Weak Not None Parenteral Weak, but Well-established
particle antigens induction TH2 cell response induced (IM) or RM greater than platform
depending for protein for several
on adjuvant subunits; commercial
requires human vaccines
repeated (hepatitis B and
vaccination HPV vaccines);
adjuvant
required
Ad5, human serotype 5 adenovirus; Ad26, human serotype 26 adenovirus; ADE, antibody-dependent enhancement; ChAd, chimpanzee adenovirus; COVID-19,
coronavirus disease 2019; HPV, human papillomavirus; IM, intramuscular; RBD, receptor-binding domain; RM, respiratory mucosal; SARS-CoV-2, severe acute
respiratory syndrome coronavirus 2; S protein, spike protein; SC, subcutaneous; TH cell, T helper cell; TRM cell, resident memory T cell; VSV, vesicular stomatitis
virus.
vaccines that entered clinical trials in China, the UK and has been reported90. Deletion of virulence factors may
the USA in mid-March 2020. Clinical trials for the therefore provide a preferred mechanism of attenuation.
remaining 24 candidates are currently recruiting For example, deletion of the 2′-O-methylase gene from
volunteers, and a couple of other candidates are also the SARS-CoV genome removes the ability of the virus to
about to enter clinical trials (TABle 2). Preclinical evaluation hide its RNA from the host cell proteins MDA5 (also
of candidate vaccines requires the use of relevant animal known as IFIH1) and IFIT1, thereby inducing a robust
models of COVID-19 (Box 3). Conventionally, the safety, antiviral response in vivo91. Another approach to viral
immunogenicity and protective efficacy of experimental attenuation is known as codon deoptimization, whereby
vaccines are rigorously evaluated and established in the nucleic acid sequence is modified to use suboptimal
animal models first before clinical trials are begun. In the codons to encode the wild-type amino acid sequence,
case of pandemic vaccine development, however, the which considerably slows the translation of the viral
preclinical and clinical stages of vaccine development are protein during infection. This approach can yield a virus
compressed and move forwards in parallel. that is highly attenuated in vivo but still able to replicate
in vitro if the correct viral protein is selected for
deoptimization92,93.
Live attenuated viral vaccines. Historically, several However, the generation of an attenuated strain of a
successful human vaccines, such as measles vaccine and the pathogen for use as a vaccine requires demonstration of its
bacillus Calmette–Guérin (BCG) vaccine for tuberculosis (TB), inability to revert genetically to become pathogenic
have been based on attenuated strains of the actual (TABle 1; Box 2).
This is particularly challenging in the case
pathogen86, with loss or mutation of virulence genes through of coronaviruses as they are known to recombine in
in vitro passage. It is now possible to rationally design nature94, and an attenuated vaccine strain could, in
attenuated virus strains by mutating or deleting virulence theory, recombine with wild coronaviruses to recreate a
genes. These deletion mutants can often replicate to a pathogenic strain. So far, there are only three attenuated
limited extent in host cells but lose the ability to cause SARS-CoV-2 vaccines generated by codon deoptimization
disease in vivo. Coronaviruses have several genes that are under preclinical development, by Mehmet Ali Aydinlar
not required for replication and that can be deleted, leading University in Turkey, Codagenix and Serum Institute of
to attenuation in vivo. Deletion of various non-structural India, and Indian Immunologicals Ltd and Griffith
proteins, as well as of the structural E protein, has been used University5.
as a strategy to engineer vaccine strains of several zoonotic
and veterinary coronaviruses87–89. Deletion of the E protein Recombinant viral-vectored vaccines. Recombinant viral-
leads to attenuation and generation of an efficacious vaccine vectored vaccines are built on either a replicationdeficient
strain87,88, but reversion of the attenuated phenotype viral backbone or an attenuated replicationcompetent viral
backbone that is bioengineered to
NAture revIeWS | IMMuNOLOgy volume 20 | october 2020 | 621
R e v i ews
Table 2 | COVID-19 vaccine candidates in or entering clinical trials
Vaccine Platform Developer Clinical Immunization Preclinical Clinical data Clinical Trial Refs
trial attributes data registrations
phase
ChAdOx1 ChAd- University Phases I–III Expressing Published Published ISRCTN89951424, 114,115
nCov-19 vectored, of Oxford, in UK, S protein; data showing data showing EudraCT 2020-001228-32,
(AZD-1222)a non- AstraZeneca South single dose or prevention of safety and good PACTR202006922165132,
replicating Africa, two repeated pneumonia induction of EudraCT 2020-001072-15,
USA and doses of IM but not neutralizing NCT04324606
Brazil injection transmission in antibodies and
NHPs T cell activation
in >90% of
vaccinees
Ad5-nCoV Ad5- CanSino Phases I Expressing NA Published data ChiCTR2000031781, 98,99
vectored, Biologics and II; S protein; showing high ChiCTR2000030906,
non- Inc., Beijing phase II single dose of dose unsafe, low NCT04341389
replicating Institute of studies in IM injection and medium
Biotechnology China and doses elicit
Canada neutralizing
antibodies
in ~50–60%
of vaccinees;
antibody levels
negatively
associated with
pre-existing
antivector
immunity and
age (>55 years)
mRNA-1273a Lipid Moderna, NIAID Phases I–III Expressing Published Published data NCT04405076, 145,146
nanoparticle– in USA S protein; report showing showing safety, NCT04283461,
mRNA two repeated induction of but highest dose NCT04470427
doses of IM neutralizing causes severe
injection antibodies and AEs in 20%
CD8+ T cells, of vaccinees;
as well as induction of
protection, in neutralizing
mouse models antibodies
in 100% of
vaccinees and
CD4+ T cell
responses in
some
126
PiCoVacc Inactivated Sinovac Biotech Phases I–III; Multiple viral Published Interim phase I/II NCT04456595,
SARS-CoV-2 phase III in antigens; data from NHP information NCT04383574,
China and two repeated model showing released NCT04352608
Brazil doses of IM protection to indicate
injection safety and
immunogenicity
NVX- Protein Novavax Phases I Recombinant Unpublished NA NCT04368988 –
CoV2373a subunit and II in S protein; information
Australia two repeated indicates
doses of IM high levels
injection of S-specific
neutralizing
antibodies
BNT162b1a Lipid BioNTech, Pfizer, Phases I–III; RBD of Published data Submitted NCT04368728, Eudra 147,148,
166
nanoparticle– Fosun Pharma dose- and S protein; from mouse report indicating CT 020-001038-36,
mRNA candidate- two repeated model showing safety, high ChiCTR2000034825
finding in doses of IM strong antibody neutralizing
Germany, injection and T cell antibody titres
USA and responses and TH1 cell-type
China CD4+ and CD8+
T cell responses
127
BBIBP-CorV Inactivated Sinopharm, Multiple viral
Phases I–III Published data Interim ChiCTR2000034780,
SARS-CoV-2 Beijing Institute in China antigens; from rodents, information ChiCTR2000032459
of Biological and United two repeated rabbits and released
Products Co. Ltd Arab doses of IM NHP models to indicate
Emirates injection showing safety and
neutralizing high antibody
antibodies and conversion rates
protection in vaccinees
622 | october 2020 | volume 20 www.nature.com/nri
R e v i ews
Table 2 (cont.) | COVID-19 vaccine candidates in or entering clinical trials
Vaccine Platform Developer Clinical Immunization Preclinical Clinical data Clinical Trial Refs
trial attributes data registrations
phase
COVID-19 Inactivated Sinopharm, Phases I–III Multiple viral NA Interim ChiCTR2000034780, –
vaccine SARS-CoV-2 Wuhan Institute in China antigens; two information ChiCTR2000031809
of Biological repeated doses released to
Products Co. Ltd of IM injection indicate safety
157
INO-4800a Plasmid DNA Inovio Phases I–III Expressing Published Interim NCT04447781,
Pharmaceuticals, in USA S protein; data showing information NCT04336410
International two repeated immunogenicity released to
Vaccine Institute doses of in mice and indicate safety
intradermal guinea pigs and overall
injection plus immune
electroporation responses
LNP- Lipid Imperial Phases I Expressing Published NA ISRCTN17072692 167
nCoVsaRNA nanoparticle– College London, and II in S protein; report showing
saRNA Morningside UK two repeated induction of
Ventures doses of IM neutralizing
injection antibodies
and TH1 cell
responses in
mouse models
COVID-19 Inactivated Chinese Phases I Multiple viral NA NA NCT04470609, –
vaccine SARS-CoV-2 Academy and II in antigens; two NCT04412538
of Medical China repeated doses
Sciences of IM injection
CVnCoV Lipid CureVac Phase I in Expressing Information NA NCT04449276 –
nanoparticle– Germany S protein; released
mRNA and two repeated suggesting
Belgium doses of IM protection in
injection animal models
Gam- Ad5- or Gameleya Phases I Single dose and NA NA NCT04436471, –
COVID-Vac Ad26- Research and II in heterologous NCT04437875
Lyo vectored, Institute Russia Ad26 prime–
non- Ad5 boost
replicating doses of IM
injection
GX-19 Plasmid DNA Genexine Phases I Expressing NA NA NCT04445389 –
Consortium and II in S protein; two
South repeated doses
Korea of IM injection
SCB-2019 Protein Clover Phase I in Trimeric Information NA NCT04405908 –
subunit Pharmaceuticals, Australia S protein; released
GlaxoSmithKline, two repeated suggesting
Dynavax doses of IM induction of
injection neutralizing
antibodies in
multiple animal
species
COVID-19 Protein Anhui Zhifei Phases I Dimeric RBD; NA NA NCT04445194, –
vaccine subunit Longcom and II in two or three NCT04466085
Biologic China repeated doses
Pharmacy, of IM injection
Chinese
Academy of
Medical Sciences
ARCoV mRNA Academy of Phase I in Expressing Information NA ChiCTR2000034112 –
Military Medical China S protein; released
Sciences, Walvax two repeated suggesting
Biotechnology, doses of IM induction of
Suzhou Abogen injection? neutralizing
Biosciences antibodies in
mice and NHPs
COVID-19 Plasmid DNA AnGes Phases I Expressing S NA NA JapicCTI-205328, –
vaccine Inc., Osaka and II in protein; two NCT04463472
University, Japan repeated doses
Takara Bio of IM injection
NAture revIeWS | IMMuNOLOgy volume 20 | october 2020 | 623
R e v i ews
Table 2 (cont.) | COVID-19 vaccine candidates in or entering clinical trials
Vaccine Platform Developer Clinical Immunization Preclinical Clinical data Clinical Trial Refs
trial attributes data registrations
phase
COVID-19 Virus-like Medicago, Laval Phase I in Multiple viral Information NA NCT04450004 –
vaccine particle University Canada antigens; released
two repeated to indicate
doses of IM antibody
injection responses in
mice
Lunar-COV19 Self- Arcturus Phases I Expressing Information NA NCT04480957 –
replicating Therapeutics, and II to S protein; released
mRNA Duke-National be laun- one dose of IM to indicate
University of ched in injection high levels of
Singapore Singapore neutralizing
antibodies after
single injection
Covaxin Inactivated Bharat Biotech, Phases I Multiple viral NA NA CTRI/2020/07/026300, –
SARS-CoV-2 Indian Council and II antigens; NCT04471519
of Medical to be two repeated
Research, launched doses of IM
National in India injection
Institute of
Virology
ZyCov-D Plasmid DNA Zydus Cadila Phases I Expressing Information NA CTRI/2020/07/026352 –
and II S protein; released
to be three repeated to indicate
launched doses of immune
in India intradermal responses in
injection several animal
species
COVID-19 Protein University of Phase I in Molecular Information Information ACTRN12620000674932p –
vaccine subunit Queensland Australia clamp- released released to
stabilized to indicate indicate safety
S protein; two neutralizing
repeated doses antibodies in
of IM injection animal models
Ad26.COV2-Sa Ad26- Johnson & Phases I Expressing Published NA NCT04436276 110
vectored, Johnson and II in S protein; data from
non- USA and two repeated NHPs showing
replicating Belgium doses of IM induction
injection of robust
neutralizing
antibodies and
protection by
single dose
KBP- Protein Kentucky Phases I Recombinant NA NA NCT04473690 –
COVID-19 subunit Bioprocessing and II in RBD-based
Inc. USA protein; two
repeated doses
of IM injection
COVID-19 VSV- Merck, IAVI Phases I Expressing NA NA – –
vaccinea vectored, and II S protein; IM
replicating to be injection
launched
in USA?
COVAX19 Protein Vaxine Pty Phase I in Recombinant NA NA NCT04453852 –
subunit Ltd, Medytox, Australia S protein with
Central Advax-SM
Adelaide Local adjuvant; single
Health Network escalating dose
of IM injection
MVC- Protein Medigen Phase I Recombinant Information NA NCT04487210 –
COV1901 subunit Vaccine to be S protein; released
Biologics, launched two repeated indicating
Dynavax in Taiwan doses of IM induction of
injection neutralizing
antibodies and
T cells
624 | october 2020 | volume 20 www.nature.com/nri
R e v i ews
Table 2 (cont.) | COVID-19 vaccine candidates in or entering clinical trials
Vaccine Platform Developer Clinical Immunization Preclinical Clinical data Clinical Trial Refs
trial attributes data registrations
phase
COVID-19 Plasmid DNA Entos Phases I Expressing Information NA – –
vaccine Pharmaceuticals and II S protein, IM released
to be injection indicating
launched induction of
in Canada neutralizing
and USA antibodies and
T cells
Ad5, human serotype 5 adenovirus; Ad26, human serotype 26 adenovirus; AEs, adverse events; ChAd, chimpanzee adenovirus; COVID-19, coronavirus disease 2019; IM,
intramuscular; NA, not available; NHP, non-human primate; RBD, receptor-binding domain; saRNA, self-amplifying RNA; SARS-CoV-2, severe acute respiratory syndrome
coronavirus 2; S protein, spike protein; TH1 cell, T helper 1 cell; VSV, vesicular stomatitis virus. aSelected for US Operation Warp Speed.
express antigens derived from the target pathogen. reduced by pre-existing immunity to Ad5, particularly in
Although only a couple of viral-vectored vaccines have elderly participants99. Depending on geographical
been approved for human use for the control of region, 35–95% of humans have significant circulating
infections such as Ebola, this platform has been widely levels of neutralizing antibodies to Ad5 (reF.103). This is
investigated and has a well-established track record for consistent with the rapidly declining antibody titres
infectious diseases and cancer, given its genetic observed in a phase II Ad5-Ebola vaccine study104. The
malleability, safety and ability to induce strong T cell vaccine is entering further advanced trials in China and
responses without the need for an adjuvant95,96. Some Canada, but the efficacy of this strategy is now in
viral vectors, such as Ad5 and ChAd, usually need to be question105. Another human adenovirus-based COVID-19
administered only once for protection and have natural vaccine, known as Ad26-S, is being developed by Johnson
tropism for the respiratory mucosa, which means they & Johnson, although there is still 40% seroprevalence for
are amenable to respiratory mucosal vaccination79. The Ad26 in humans106. As Ad26 is inherently less
technology already exists for their large-scale clinical immunogenic than Ad5 (reF.107), effective immunity
grade production and storage. requires repeated homologous or heterologous
Thus, recombinant viral vectors are the second vaccination, as has been shown in Ad26-HIV and Ad26-
most common platform for COVID-19 vaccine Ebola vaccine studies in humans108,109. Nevertheless, a
development, with 4 candidates currently in clinical single parenteral administration of an Ad26-vectored
trials (TABle 2), 38 under preclinical development5 and 3 COVID-19 vaccine (Ad26.COV2.S) offered robust
(ChAdOx1 nCoV-19, Ad26-S and VSV-S) selected for protection in a non-human primate model of SARS-CoV-2
Us operation Warp speed97 (TABle 2). The non-replicating (reF.110).
viral platforms are mostly based on Ad5 or MVA, and ChAdOx1 nCoV-19 (also known as AZD-1222), which is
most of these vaccine candidates express the S protein being developed by Oxford University, UK, and
or RBD of SARS-CoV-2. Replication-competent viral AstraZeneca, is the most clinically advanced COVID-19
vectors are mainly based on the vaccine strains of other vaccine (TABle 2). Humans have low seroprevalence for
human pathogens (such as measles or influenza viruses) ChAd, hence its strong immunogenicity and utility for
or veterinary pathogens (such as vesicular stomatitis heterologous prime–boost COVID-19 vaccination79,107,111.
virus (VSV)). However, it will be important to consider The development of ChAdOx1 nCoV-19 is based on
whether humans have pre-existing immunity against the promising human studies with ChAdOx1-MERS vaccine112
viral backbone (TABle 1). Pre-existing antibodies can impair and ChAdOx1-TB vaccine113. However, although
the ability of such vaccines to engage the immune intramuscular delivery of ChAdOx1 nCoV-19 reduced
system. Use of viral backbones such as ChAd, for which SARS-CoV-2 viral load in the lungs and prevented
humans have little to no pre-existing immunity, can help pneumonia in rhesus macaques, it did not reduce viral
to circumvent this issue79. loads in the upper respiratory tract114. A recently
Ad5-nCOV, which is being developed by the reported phase I/II study shows its safety and the
Chinese vaccine company CanSino Biologics, is induction of potent neutralizing antibody and T cell
designed to induce neutralizing antibodies to SARS- responses following a single parenteral injection, which
CoV-2 S protein following intramuscular injection are boosted further by a second homologous vaccination
(TABle 2). Without published preclinical data, it entered 115. It remains unclear from this trial to what extent both
US Operation Warp Speed phase I/II clinical trials with three doses of vaccine tested CD4+ and CD8+ T cell subsets were activated.
A public–private partnership 98,99. Of note, these doses are 10–30 times higher than
initiated and funded by the Us
those used in previous trials of intramuscular vaccines100 VSV-S is a replication-competent COVID-19 vaccine
government to accelerate and
–102. Whereas the highest dose generated unacceptable under development by Merck116 and other groups.
coordinate the
development, manufacture and toxicity and was dropped from the phase II study99, the Merck’s vaccine is built upon the licensure of its highly
distribution of coronavirus smaller doses induced S protein-specific neutralizing efficacious VSV-Ebola vaccine, which induces neutralizing
disease 2019 (CoViD-19) vaccines,
antibodies in only 50% of the vaccine recipients98. The antibodies and cellular immunity against Ebola virus
therapeutics and diagnostics. it
phase II study largely reaffirms the phase I observations surface glycoprotein117. VSV is a veterinary virus to which
was introduced by the Trump
administration in early April 2020. that, although the vaccine induces both antibody and T humans have no pre-existing immunity. However, the
cell responses, its potency is cloning capacity of the VSV vector is
NAture revIeWS | IMMuNOLOgy volume 20 | october 2020 | 625
R e v i ews
by Chinese state-owned Sinopharm, was tested in a
Box 3 | Animal models of COVID-19 for vaccine testing
range of animal models, with demonstrated efficacy in
there is an urgent need to identify suitable animal models for the preclinical evaluation of non-human primates127. Although these findings provide
coronavirus disease 2019 (covID-19) vaccines182. A large number of animal species have optimism, the observations were made in rather short-
differing degrees of susceptibility to severe acute respiratory syndrome coronavirus 2 (SArS-
term studies and should be interpreted with caution.
cov-2) infection, depending on the relative binding affinity of the virus to the host angiotensin-
converting enzyme 2 (Ace2) receptor or on host protease activities on the S protein183.
Inactivated viral vaccines often require an adjuvant
Among the animal species tested, Ace2 of rhesus macaques has the greatest binding and repeated administration to be effective (TABle 1). The
activity for SArS-cov-2 (reF.183). Infected macaques shed SArS-cov-2 from the upper and the use of alum as an adjuvant126,127 makes them unsuitable
lower respiratory tract but they do not develop the same clinical signs and age-dependent for respiratory mucosal delivery128. Although the
disease severity as humans184,185. cats, ferrets and hamsters are also susceptible to SArS-cov-2 protection mediated by intramuscular immunization with
infection. Notably, natural airborne and contact transmissions of SArS-cov-2 have been PiCoVacc or BBIBP-CorV indicates some level of mucosal
reported in cats and hamsters, respectively, but not in ferrets186. Hamsters, but not cats and immunity, probably through the transport of systemic
ferrets, manifest severe clinical symptoms. thus, these animal models are differentially antibodies to the lungs, the durability of such immunity
capable of recapitulating relevant aspects of covID-19.
remains unclear as SARS-CoV-2 challenge was performed
1–4 weeks after vaccination126,127. Furthermore, similarly
mouse models are widely used for vaccine testing owing to their affordability and the
to protein subunit vaccines, inactivated viral vaccines are
availability of immunoreagents and transgenic mouse strains. However, the Ace2 of
conventional mice does not bind well to SArS-cov S protein187. transgenic mice expressing poor inducers of cytotoxic CD8+ T cells, which are likely to
human Ace2 were initially developed and thoroughly characterized for the study of SArS-cov be required for an effective COVID-19 vaccine.
and have now been shown to support SArS-cov-2 replication in the lung, and these mice
develop interstitial pneumonia similar to humans188. Human Ace2-expressing mice that are Studies with inactivated SARS-CoV and respiratory
further humanized to express human HlA genes and/or to have human immune cells will be syncytial virus vaccines have reported vaccine-related
useful for studying human immune responses and immunodominant epitopes following enhancement of disease, likely involving a TH2 cell
vaccination and viral infection with SArS-cov-2. beyond animal models, of further relevance to response and lung eosinophilia, which may be worsened
human applications is the ongoing ethical debate regarding intentional challenge of
in aged hosts56,74,129. Although PiCoVacc or BBIBP-CorV
vaccinated young people with SArS-cov-2.
did not worsen lung disease within 7 days after infection,
alum is known to drive TH2 cell-mediated immune
responses, which warrants further safety investigations.
limited to 4kb, and its suitability for respiratory mucosal The use of TH1 cell-skewing modified alum or other
vaccination is unclear. A single parenteral vaccination adjuvants such as CpG may avert such safety concerns130,
with a VSV vector expressing S protein provides 131.
protection against SARS-CoV-2 in both mouse and
hamster models118,119. Among other viral-vectored Protein subunit vaccines. Currently, there are seven
candidates is non-replicating MVA. MVA has widely been COVID-19 subunit vaccines in clinical trials (TABle 2), with
explored as a vaccine carrier and has a cloning capacity 50 other candidates under preclinical development,
of up to 30kb. However, as it is not robustly making this the most common platform5. Subunit
immunogenic, MVA is often used as a booster vaccine or vaccines primarily induce CD4+ TH cell and antibody
repeated injection is required to be effective, as was the responses. Therefore, most of these vaccines contain
case in clinical testing of an MVA-MERS-S vaccine120. full-length SARS-CoV-2 S protein or portions of it with the
goal of inducing neutralizing antibodies, similarly to the
Inactivated viral vaccines. Physically or chemically majority of SARS and MERS vaccines, which had differing
inactivated viruses have been used successfully in levels of efficacy132–134.
human vaccines against polio, hepatitis A and influenza Subunit vaccines can be designed to focus the immune
121,122. Inactivated viruses can be rapidly generated and response towards neutralizing epitopes, thereby averting the
scaled up in a pandemic situation using well-established production of non-neutralizing antibodies that may promote
infrastructure and methods123. Inactivated viral vaccines ADE of disease135. However, unlike nucleic acid-based or
have few safety concerns, unlike their live attenuated viral-vectored vaccines, recombinant S proteins in subunit
counterparts, and they express a wide range of native vaccines could have an improper epitope conformation
viral antigens, including surface antigens with retained unless they are produced in mammalian cells136. Proteins or
epitope conformations that can induce conformation- peptides alone are poorly immunogenic and generally
dependent antibody responses124,125. require not only an adjuvant but also repeated
Currently, there are five early clinical trials to assess administration, and they are poor activators of CD8+ T cell
inactivated SARS-CoV-2 vaccines (TABle 2), with an responses (TABle 1). Furthermore, this platform is generally
additional nine candidates in preclinical development5. unsuitable for respiratory mucosal vaccination. As is the case
PiCoVacc, an inactivated SARS-CoV-2 and alum- for inactivated viral vaccines, use of unmodified alum as an
adjuvanted vaccine developed by Sinovac Biotech Ltd in adjuvant skews the immune response towards TH2 cell-like
China, is the most advanced candidate with published responses56, which is undesirable for host defence against
preclinical results126. It protects rhesus macaques against SARS-CoV-2 and may have a role in ADE of disease74,130. In
SARS-CoV-2, with reduced viral titres and this regard, subunit COVID-19 vaccines being developed by
immunopathology associated with antibodies to S GlaxoSmithKline and Novavax use AS03 and Matrix-M
protein and nucleocapsid126. BBIBP-CorV, another adjuvants, respectively5.
inactivated virus candidate, which is being developed
626 | october 2020 | volume 20 www.nature.com/nri
R e v i ews
Virus-like particles. VLPs are spontaneously forming doses of two repeated parenteral injections are generally
particles composed of several structural viral proteins safe and induce strong S protein-specific antibody
that are co-expressed or admixed. Several commercial responses and a primarily CD4+ T cell response in most
vaccines, such as hepatitis B and human papillomavirus trial participants146. Pfizer and BioNTech are also
vaccines, are based on VLPs137. In the case of enveloped assessing an mRNA–lipid nanoparticle vaccine encoding
coronaviruses, VLPs form when the viral proteins S, M the S protein RBD (known as BNT162b1) in humans, who
and E, with or without N, are co-expressed in eukaryotic developed robust S protein-specific antibody and CD4+
producer cells138,139. This results in active budding from and CD8+ T cell responses following two repeated parenteral
the producer cells of VLPs that are structurally identical injections147,148. The Pfizer/BioNTech and Moderna vaccines
to the infectious virus but lack the viral genome and thus have both been selected for US Operation Warp
are non-infectious. The presence of S protein on the Speed97 (TABle 2).
surface of VLPs enables them to bind and enter ACE2+ Although no mRNA vaccine has yet been licensed for
cells in the same manner as the parent virus140. Unlike human use, their potential is supported by previous
subunit vaccines, the array of S protein on the VLP studies of influenza, rabies and Zika virus infections in
surface crosslinks the B cell receptor and directly animals149–153. For example, an mRNA vaccine for
activates B cells, but, like subunit and inactivated viral influenza virus induced long-termhumoral immunity in
vaccines, VLPs also typically require an adjuvant and young and aged mice149, and an mRNA vaccine for Zika
repeated administration137. Notwithstanding this, the virus induced both antibodies and cytotoxic CD8+ T cells
VLP technology is well established, the biology and in mice154. However, two clinical studies show disparities
safety of coronavirus VLPs are understood and their in the magnitude and longevity of immune responses
large-scale production to Good Manufacturing Practice induced by mRNA vaccines152,155. Thus, although mRNA-
standards is relatively straightforward. based COVID-19 vaccines show promise from early
Currently, there is only 1 VLP-based COVID-19 vaccine clinical testing, questions remain about their protective
in clinical trials (TABle 2), with 12 more under preclinical efficacy in humans. It is also unclear whether mRNA
development5. These are produced either in vivo from a vaccines are amenable to respiratory mucosal delivery.
viral vector, such as MVA, that expresses the VLP Plasmid DNA vaccines share several characteristics
components (a platform being developed by GeoVax) or with mRNA vaccines, including safety, ease of production
more often in vitro from producer cells. Notably, and scalability156. However, they are poorly
Medicago, a Canadian company, produces its SARS- immunogenic, requiring multiple doses and the addition
CoV-2 VLPs from genetically engineered plants. Its of an adjuvant. Currently, there are four plasmid DNA-
unpublished results seem to suggest efficacy in inducing based COVID-19 vaccines in clinical testing (TABle 2), with
neutralizing antibodies in mice141. 11 more under preclinical development. INO-4800, a
plasmid DNA vaccine expressing SARS-CoV-2 S protein, is
Nucleic acid-based vaccines. Recombinant plasmid being developed by the US biotech company Inovio
DNA has been explored as a vaccine platform for Pharmaceuticals. A preclinical study in mice and guinea
decades, whereas mRNA has emerged more recently as pigs examined the immunogenicity of this vaccine but
a promising platform142,143. Currently, there are 6 mRNA- did not provide any data pertaining to protection against
based COVID-19 vaccines and 4 DNA-based COVID-19 challenge157. Two repeated injections of an S protein-
vaccines in clinical trials (TABle 2), with 27 such vaccines expressing plasmid DNA vaccine resulted in robust
(16 mRNA-based and 11 DNA-based vaccines) under protective immunity in rhesus macaques158.
preclinical development5.
The antigen-encoding mRNA complexed with a Conclusions and outlook
carrier such as lipid nanoparticles can be efficiently The world is in dire need of safe, effective COVID-19
delivered in vivo into the cytoplasm of host cells for vaccine strategies. Many laboratories and companies
protein translation and post-translational modifications have scrambled to rapidly develop these vaccines,
142,144, which is an advantage over recombinant protein resulting in more than 160 vaccine candidates, with a
subunit vaccines. mRNA vaccines are non-infectious and handful having entered phase I, II and III clinical trials
are synthesized by in vitro transcription, free of microbial within a short period of 6 months. Although we are just
molecules. These beneficial features differentiate mRNA beginning to understand COVID-19 and its vaccine
vaccines from live attenuated viral vaccines, inactivated requirements, most of the advanced vaccine platforms
viral vaccines, subunit vaccines and recombinant viral- have been extensively explored for other infections and
vectored vaccines in terms of safety, efficacy and issues cancer79,95,96,159. While it is important to pursue various
of antivector immunity, enabling their rapid and vaccine strategies in parallel, it is equally important not
inexpensive production and repeated vaccination142 (TABle to lose sight of this existing scientific knowledge to make
1). well-informed decisions around which strategies to
mRNA-1273, which is produced by Moderna, an prioritize.
American biotech company that has experience with The various vaccine platforms and strategies have
mRNA-based MERS vaccines, encodes a their immunological pros and cons (TABle 1), but modern
prefusionstabilized SARS-CoV-2 S protein encapsulated in immunological principles and data from prior studies of
lipid nanoparticles. It entered clinical testing even before similar platforms lead us to surmise that a parenteral
the release of preclinical data145. Recently published COVID-19 vaccine strategy capable of inducing a robust,
phase I clinical trial data indicate that low and medium durable response involving both neutralizing antibodies
NAture revIeWS | IMMuNOLOgy volume 20 | october 2020 | 627
R e v i ews
Priority vaccination
A ‘pandemic vaccine’ or a vaccine
• Health-care workers
fully validated from the
• Individuals with co-morbidities
‘rationalized vaccine pipeline’ to be
• Seniors
offered to high-risk populations first
• Ethnic minorities
owing to limited supplies
Other groups to consider
for vaccination
• Individuals infected with SARS-CoV-2 but
• SARS-CoV-2 exposed who developed poor immunity
• Waning immunity • Those who initially developed
immunity but it waned very quickly
Individuals vaccinated with a
• Pandemic-vaccinated candidate vaccine from the
• Waning immunity ‘pandemic pipeline’ that offers
poor or short-lived immunity
Mass vaccination
• The best vaccine strategies
identified from the rationalized
• National vaccine paradigm
• Continental • Regional immunization owing to
• Global limited distribution
• Worldwide immunization
Pandemic vaccine paradigm
1–2 years
Rationalized vaccine paradigm
10–15 years
Fig. 2 | Evolving scenarios for global COVID-19 vaccine development and vaccination of high-risk populations such as health-care workers, seniors,
demand. In response to the urgent demand for a vaccine, more than two people with co-morbidities and ethnic minorities, who have been
dozen candidate vaccines are advancing through clinical trials following an disproportionately affected by COVID-19, when vaccine supply is initially
expedited pandemic vaccine development paradigm, withmany steps of the limited. Aside from these prioritized groups, it may also be necessary to
development process occurring in parallel before a successful outcome of consider that asymptomatic individuals, patients who have recovered from
previous steps has been confirmed. Vaccine candidates will continue to be COVID-19 but generated poor immunity or whose immunity quickly waned,
preclinically and clinically evaluated following conventional and/or and individuals who received a rapidly developed ‘pandemic’ vaccine that
rationalized vaccine development processes over the next few years. These provided suboptimal protection or rapidly waning immune responses may
efforts will evolve to meet the demands for vaccination in several likely require a booster vaccination to ensure sufficient levels of population
scenarios that are predicted on the basis of sociopolitical challenges and the protection for herd immunity. Ultimately, regional, continental and global
emerging data regarding the trajectory of the coronavirus disease 2019 populations will be subject to mass vaccination programmes based on the
(COVID-19) pandemic and the host response to severe acute respiratory extent of national and global vaccine distribution and also likely according
syndrome coronavirus 2 (SARS-CoV-2). One scenario is the priority to the relative regional severity of outbreaks.
and T cells should provide a significant level of protection. vaccine strategy capable of inducing these responses
Almost all of the current vaccines in the human directly in the respiratory mucosa will be most effective
immunization programme are delivered via the skin or in the early control or clearance of SARS-CoV-2. This is
muscle, and most of the current COVID-19 vaccine strategies particularly relevant to high-risk elderly populations, who
also focus on the parenteral route of vaccination will require a particularly robust vaccine strategy. In this
(TABle 2). We further surmise that a respiratory mucosal regard, a respiratory mucosal vaccine strategy for
628 | october 2020 | volume 20 www.nature.com/nri
R e v i ews
COVID-19 may draw on the successful experience in with preclinical efficacy data but limited clinical data to
respiratory mucosal delivery of influenza, measles and high-risk populations may be necessary (Fig. 2).
TB vaccines to humans160–162. Respiratory mucosal The evolving process of vaccine development will
vaccination also has the advantages of being needle-free continue over the next few years until more clinical trials are
and requiring a much smaller dose than the parenteral completed, additional vaccine strategies are evaluated and
route. However, compared with the parenteral route, host defence against SARS-CoV-2, including postinfection
fewer vaccine platforms are safe and effective for immunity, is better understood (Fig. 2). Probably not until then
respiratory mucosal vaccination. Furthermore, the use of will global mass immunization become a reality. It is possible
inhalational devices for respiratory mucosal delivery may that the populations that receive the first round of vaccines
potentially be a limiting factor for widespread will have waning immunity and require boosting using
application in resource-poor settings. improved second-generation COVID-19 vaccines.
According to the pandemic vaccine development Furthermore, in addition to unexposed individuals, some
paradigm (Fig. 2), the conventional vaccine development individuals who have recovered from COVID-19 who develop
milestones are compressed from a time frame of 10–15 poor or waning immunity may also require vaccination163.
years to 1–2 years, with overlapping preclinical, clinical and
scale-up manufacturing processes occurring in parallel6. Given the challenges in resources, manufacturing and
Owing to the accelerated development process, the interim issues associated with distribution and regional
data from ongoing clinical and preclinical vaccine studies are protectionism, the implementation of vaccination
being published almost in real time. As a result, crucial programmes will likely be uneven, asynchronous and
information about the longevity and quality of vaccine- variable — involving different vaccine platforms and
induced protective immunity is unavailable. As transmission strategies around the globe164,165. In this regard, some
rates and the numbers of new cases have reduced in many resource-rich countries have already secured large numbers
countries, it is uncertain whether the phase II and phase III of doses of different candidate vaccines without knowing
studies of the front-runner candidates will reach a reliable which one may prove effective. The heated debate has
conclusion with regard to their protective efficacy. begun globally over who should be at the front of the line
Furthermore, these vaccine candidates have been studied in when vaccine supply is limited. The founding of the
isolation, which makes it difficult to directly compare the COVID-19 Vaccines Global Access (COVAX) Facility by Gavi,
effectiveness of different candidates. Thus, it would be the Coalition for Epidemic Preparedness Innovations (CEPI)
premature to hail the safety and immunogenicity observed and the WHO is an attempt to garner resources and unite
in COVID-19 vaccine trials as a real success. To a large extent, higher- and lower-income countries for the coordinated,
such outcomes could be anticipated from past studies rapid, transparent and equitable access to COVID-19
testing the same platforms and delivery routes. vaccines worldwide.
Nevertheless, rapid deployment of a vaccine
Published online 4 September 2020
1. World Health Organization. WHO coronavirus disease responses, including antibody responses, in dendritic cell responses and, subsequently, delayed T
(COVID-19) dashboard. WHO https://covid19.who.int/ asymptomatic individuals are not only lower but also cell activation in infected individuals.
(2020). decrease faster during the convalescent phase. 19. Remy, K. E. et al. Severe immunosuppression and not a
2. Chou, R. et al. Epidemiology of and risk factors for 10. Sungnak, W. et al. SARS-CoV-2 entry factors are highly cytokine storm characterize COVID-19 infections.
coronavirus infection in health care workers. Ann. Intern. expressed in nasal epithelial cells together with innate JCI Insight https://doi.org/10.1172/jci.insight.140329
Med. https://doi.org/10.7326/M20-1632 (2020). immune genes. Nat. Med. 26, 681–687 (2020). (2020).
3. Flaxman, S. et al. Estimating the effects of 11. Zou, X. et al. Single-cell RNA-seq data analysis on the 20. Blanco-Melo, D. et al. Imbalanced host response to
nonpharmaceutical interventions on COVID-19 in receptor ACE2 expression reveals the potential risk of SARS-CoV-2 drives development of COVID-19. Cell 181
Europe. Nature 584, 257–261 (2020). different human organs vulnerable to 2019-nCoV , 1036–1045.e9 (2020).
4. Sanche, S. et al. High contagiousness and rapid spread of infection. Front. Med. 14, 185–192 (2020). 21. Merad, M. & Martin, J. C. Pathological inflammation in
severe acute respiratory syndrome coronavirus 2. Emerg. 12. Hoffmann, M. et al. SARS-CoV-2 cell entry depends on patients with COVID-19: a key role for monocytes and
Infect. Dis. 26, 1470–1477 (2020). ACE2 and TMPRSS2 and is blocked by a clinically proven macrophages. Nat. Rev. Immunol. 20, 355–362 (2020).
5. World Health Organization. Draft landscape of COVID-19 protease inhibitor. Cell 181, 271–280.e8 (2020).
candidate vaccines. WHO https://www.who. int/ 22. Zhou, Y. et al. Pathogenic T-cells and inflammatory
publications/m/item/draft-landscape-of-covid-19- This is one of the first studies to identify ACE2 and monocytes incite inflammatory storms in severe
candidate-vaccines (2020). TMPRSS2 as the cell surface receptor molecules used COVID-19 patients. Natl Sci. Rev. 7, 998–1002 (2020).
6. Lurie, N., Saville, M., Hatchett, R. & Halton, J. by SARS-CoV-2 for infection.
Developing Covid-19 vaccines at pandemic speed. 13. Sallenave, J.-M. & Guillot, L. Innate immune signaling and 23. Zhou, F. et al. Clinical course and risk factors for mortality
N. Engl. J. Med. 382, 1969–1973 (2020). This article proteolytic pathways in the resolution or of adult inpatients with COVID-19 in Wuhan, China: a
describes the differences between the pandemic exacerbation of SARS-CoV-2 in Covid-19: key therapeutic retrospective cohort study. Lancet 395, 1054–1062
vaccine development and the conventional targets? Front. Immunol. 11, 1229 (2020). (2020).
rationalized vaccine development paradigms 14. Puelles, V. G. et al. Multiorgan and renal tropism of SARS- 24. Liao, M. et al. Single-cell landscape of bronchoalveolar
and timelines. CoV-2. N. Engl. J. Med. 383, 590–592 (2020). immune cells in patients with COVID-19. Nat. Med. 26,
7. Chau, N. V. V. et al. The natural history and transmission 15. de Wit, E., van Doremalen, N., Falzarano, D. & Munster, 842–844 (2020).
potential of asymptomatic SARS-CoV-2 infection. Clin. V. J. SARS and MERS: recent insights into emerging 25. Fulop, T. et al. Immunosenescence and inflamm-aging as
Infect. Dis. https://doi.org/10.1093/cid/ciaa711 (2020). coronaviruses. Nat. Rev. Microbiol. 14, 523–534 two sides of the same coin: friends or foes? Front.
8. Poletti, P. et al. Probability of symptoms and critical (2016). Immunol. 8, 1960 (2017).
disease after SARS-CoV-2 infection. Preprint at arXiv 16. Prompetchara, E., Ketloy, C. & Palaga, T. Immune responses 26. Haq, K. & McElhaney, J. E. Immunosenescence:
https://arxiv.org/abs/2006.08471 (2020). Chau et al. in COVID-19 and potential vaccines: lessons learned from influenza vaccination and the elderly. Curr. Opin.
(2020) and Poletti et al. indicate high rates of SARS and MERS epidemic. Asian Pac. J. Allergy Immunol. Immunol. 29, 38–42 (2014).
asymptomatic individuals following SARS-CoV-2 38, 1–9 (2020). Fulop et al. (2017) and Haq and McElhaney discuss a
exposure. 17. Sariol, A. & Perlman, S. Lessons for COVID-19 immunity unique challenge for developing effective and safe
9. Long, Q.-X. et al. Clinical and immunological from other coronavirus infections. Immunity https:// vaccine strategies for seniors, who are among those
assessment of asymptomatic SARS-CoV-2 infections. doi.org/10.1016/j.immuni.2020.07.005 (2020). most in need of vaccine-mediate immune protection
Nat. Med. 26, 1200–1204 (2020). 18. Zhou, R. et al. Acute SARS-CoV-2 infection impairs dendritic from COVID-19, and suggest that vaccine-induced T
This study provides evidence that asymptomatic cell and T cell responses. Immunity 53, 1–14 (2020). cell immunity is more important than antibody
individuals infected with SARS-CoV-2 can shed the responses in seniors.
virus for a significantly longer time than their This study documents SARS-CoV-2-mediated innate 27. Tay, M. Z., Poh, C. M., Rénia, L., MacAry, P. A. & Ng, L.
symptomatic counterparts and that immune immune suppression associated with impaired F. P. The trinity of COVID-19: immunity,
NAture revIeWS | IMMuNOLOgy volume 20 | october 2020 | 629
R e v i ews
inflammation and intervention. Nat. Rev. Immunol. antibodies with a vaccine that induces both 67. Chakraborty, S. et al. Symptomatic SARS-CoV-2
20, 363–374 (2020). neutralizing antibodies and T cell-mediated infections display specific IgG Fc structures.
28. Zhao, J. et al. Antibody responses to SARS-CoV-2 in immunity, including vaginal TRM cells, and describes Preprint at medRxiv https://doi.org/10.1101/
patients of novel coronavirus disease 2019. Clin. the importance of protective T cells, particularly 2020.05.15.20103341 (2020).
Infect. Dis. https://doi.org/10.1093/cid/ciaa344 (2020). when neutralizing antibody levels are suboptimal. 68. Lee, N. et al. Anti-SARS-CoV IgG response in relation to
This study lends further support to including robust disease severity of severe acute respiratory
29. Ni, L. et al. Detection of SARS-CoV-2-specific humoral and T cell responses in the design of COVID-19 vaccine syndrome. J. Clin. Virol. 35, 179–184 (2006).
cellular immunity in COVID-19 convalescent individuals. strategies. 69. Liu, L. et al. Anti-spike IgG causes severe acute lung injury
Immunity 52, 971–977.e3 (2020). 50. Zhao, J., Zhao, J. & Perlman, S. T cell responses are by skewing macrophage responses during acute SARS-
30. Grifoni, A. et al. Targets of T cell responses to SARS- required for protection from clinical disease and for CoV infection. JCI Insight 4, e123158 (2019).
CoV-2 coronavirus in humans with COVID-19 disease virus clearance in severe acute respiratory syndrome 70. Eroshenko, N. et al. Implications of antibodydependent
and unexposed individuals. Cell 181, 1489–1501.e15 coronavirus-infected mice. J. Virol. 84, 9318–9325 enhancement of infection for SARS-CoV-2
(2020). (2010). countermeasures. Nat. Biotechnol. 38, 789–791 (2020).
31. Shen, C. et al. Treatment of 5 critically ill patients with 51. Turner, D. L. et al. Lung niches for the generation and
COVID-19 with convalescent plasma. JAMA 323, 1582 maintenance of tissue-resident memory T cells. 71. Weingartl, H. et al. Immunization with modified vaccinia
(2020). Mucosal Immunol. 7, 501–510 (2014). virus Ankara-based recombinant vaccine against severe
32. Seow, J. et al. Longitudinal evaluation and decline of 52. Jeyanathan, M., Yao, Y., Afkhami, S., Smaill, F. & Xing, Z. acute respiratory syndrome is associated with enhanced
antibody responses in SARS-CoV-2 infection. New tuberculosis vaccine strategies: taking aim at un- hepatitis in ferrets. J. Virol. 78, 12672–12676 (2004).
Preprint at medRxiv https://doi.org/10.1101/ natural immunity. Trends Immunol. 39, 419–433
2020.07.09.20148429 (2020). (2018). 72. Czub, M., Weingartl, H., Czub, S., He, R. & Cao, J.
This study follows the kinetic changes in neutralizing This recent review highlights the major Evaluation of modified vaccinia virus Ankara based
antibody levels up to 94 days after the onset of immunological differences and protective outcomes recombinant SARS vaccine in ferrets. Vaccine 23,
COVID-19 symptoms; it finds that antibody levels are between parenteral and respiratory mucosal routes 2273–2279 (2005).
positively correlated with the severity of disease and of vaccination and suggests ways in which to induce 73. Kam, Y. W. et al. Antibodies against trimeric S
decline rapidly, bringing into question the value of holistic mucosal immunity to mucosal pathogens. glycoprotein protect hamsters against SARS-CoV
serological assessment and the role of such 53. Haddadi, S. et al. Mucosal-pull induction of lung-resident challenge despite their capacity to mediate
neutralizing antibodies in herd immunity. memory CD8 T cells in parenteral TB vaccine-primed FcγRIIdependent entry into B cells in vitro. Vaccine
33. Walls, A. C. et al. Structure, function, and antigenicity of hosts requires cognate antigens and CD4 T Cells. Front. 25, 729–740 (2007).
the SARS-CoV-2 spike glycoprotein. Cell 181, 281–292.e6 Immunol. 10, 2075 (2019). 74. Diamond, M. S. & Pierson, T. C. The challenges of
(2020). vaccine development against a new virus during a
34. Pinto, D. et al. Cross-neutralization of SARS-CoV-2 by a 54. Zhao, J. et al. Airway memory CD4+ T cells mediate pandemic. Cell Host Microbe 27, 699–703 (2020).
human monoclonal SARS-CoV antibody. Nature 583, protective immunity against emerging respiratory
290–295 (2020). coronaviruses. Immunity 44, 1379–1391 (2016). 75. Buchholz, U. J. et al. Contributions of the structural
35. Jiang, S., Hillyer, C. & Du, L. Neutralizing antibodies 55. Janice Oh, H.-L., Ken-En Gan, S., Bertoletti, A. & Tan, Y.-J. proteins of severe acute respiratory syndrome
against SARS-CoV-2 and other human coronaviruses. Understanding the T cell immune response in SARS coronavirus to protective immunity. Proc. Natl Acad.
Trends Immunol. 41, 355–359 (2020). coronavirus infection. Emerg. Microbes Infect. 1, 1–6 Sci. 101, 9804–9809 (2004).
36. Duan, J. et al. A human SARS-CoV neutralizing antibody (2012). 76. Stephensen, C. B., Casebolt, D. B. & Gangopadhyay, N. N.
against epitope on S2 protein. Biochem. Biophys. 56. Bolles, M. et al. A double-inactivated severe acute Phylogenetic analysis of a highly conserved region of
Res. Commun. 333, 186–193 (2005). respiratory syndrome coronavirus vaccine provides the polymerase gene from 11 coronaviruses and
37. Coughlin, M. et al. Generation and characterization of incomplete protection in mice and induces increased development of a consensus polymerase chain reaction
human monoclonal neutralizing antibodies with eosinophilic proinflammatory pulmonary response assay. Virus Res. 60, 181–189 (1999).
distinct binding and sequence features against SARS upon challenge. J. Virol. 85, 12201–12215 (2011).
coronavirus using XenoMouse®. Virology 361, 93–102 57. Tseng, C.-T. et al. Immunization with SARS coronavirus 77. Gao, Y. et al. Structure of the RNA-dependent RNA
(2007). vaccines leads to pulmonary immunopathology on polymerase from COVID-19 virus. Science 368, 779–
38. To, K. K. W. et al. Temporal profiles of viral load in challenge with the SARS virus. PLoS ONE 7, e35421 782 (2020).
posterior oropharyngeal saliva samples and serum (2012). 78. Rauch, S., Jasny, E., Schmidt, K. E. & Petsch, B. New
antibody responses during infection by SARS-CoV-2: an 58. Braun, J. et al. SARS-CoV-2-reactive T cells in healthy vaccine technologies to combat outbreak
observational cohort study. Lancet Infect. Dis. 20, 565– donors and patients with COVID-19. Nature https:// situations. Front. Immunol. 9, 1963 (2018).
574 (2020). doi.org/10.1038/s41586-020-2598-9 (2020). 79. Afkhami, S., Yao, Y. & Xing, Z. Methods and clinical
39. Liu, W. et al. Evaluation of nucleocapsid and spike development of adenovirus-vectored vaccines against
protein-based enzyme-linked immunosorbent assays 59. Ahmed, S. F., Quadeer, A. A. & McKay, M. R. Preliminary mucosal pathogens. Mol. Ther. Methods Clin. Dev. 3,
for detecting antibodies against SARS-CoV-2. J. Clin. identification of potential vaccine targets for the 16030 (2016).
Microbiol. 58, e00461-20 (2020). COVID-19 coronavirus (SARS-CoV-2) based on SARS-CoV 80. Moreno-Fierros, L., García-Silva, I. & Rosales-Mendoza, S.
40. Long, Q. X. et al. Antibody responses to SARS-CoV-2 in immunological studies. Viruses 12, 254 (2020). Development of SARS-CoV-2 vaccines: should we focus
patients with COVID-19. Nat. Med. 26, 845–848 (2020). on mucosal immunity? Expert. Opin. Biol. Ther. 20, 831–
60. Mateus, J. et al. Selective and cross-reactive SARS-CoV-2 T 836 (2020).
41. Nakanaga, K., Yamanouchi, K. & Fujiwara, K. Protective cell epitopes in unexposed humans. Science https:// 81. Belyakov, I. M. & Ahlers, J. D. What role does the route
effect of monoclonal antibodies on lethal mouse doi.org/10.1126/science.abd3871 (2020). of immunization play in the generation of
hepatitis virus infection in mice. J. Virol. 59, 168–171 61. Le Bert, N. et al. SARS-CoV-2-specific T cell immunity in protective immunity against mucosal pathogens?
(1986). cases of COVID-19 and SARS, and uninfected controls. J. Immunol. 183, 6883–6892 (2009).
42. Lecomte, J. et al. Protection from mouse hepatitis virus Nature https://doi.org/10.1038/s41586- 020-2550-z 82. Szabo, P. A., Miron, M. & Farber, D. L. Location,
type 3-induced acute disease by an antinucleoprotein (2020). location, location: tissue resident memory T cells in
monoclonal antibody. Arch. Virol. 97, 123–130 (1987). Braun et al. (2020), Mateus et al. (2020) and Le Bert et mice and humans. Sci. Immunol. 4, eaas9673
al. consistently find the presence, in a significant (2019).
43. Yu, H. et al. Distinct features of SARS-CoV-2-specific IgA proportion of uninfected individuals, of memory CD4+ 83. Xing, Z. et al. Innate immune memory of tissueresident
response in COVID-19 patients. Eur. Respir. J. https:// T cells cross-reactive to SARS-CoV-2, likely resulting macrophages and trained innate immunity: re-vamping
doi.org/10.1183/13993003.01526-2020 (2020). from previous exposure to common cold vaccine concept and strategies. J. Leukoc. Biol. https://
coronaviruses as well as animal coronaviruses. These doi.org/10.1002/JLB.4MR0220-446R (2020).
44. Padoan, A. et al. IgA-Ab response to spike findings offer a potential mechanism underlying
glycoprotein of SARS-CoV-2 in patients with differential susceptibility to SARS-CoV-2 infection and 84. Netea, M. G. et al. Trained immunity: a tool for
COVID-19: a longitudinal study. Clin. Chim. Acta suggest that a COVID-19 vaccine may boost such pre- reducing susceptibility to and the severity of SARS-
507, 164–166 (2020). existing cross-reactive memory CoV-2 infection. Cell 181, 969–977 (2020).
45. Cao, W.-C., Liu, W., Zhang, P.-H., Zhang, F. & Richardus, J. T cells in some individuals. 85. Yao, Y. et al. Induction of autonomous memory alveolar
H. Disappearance of antibodies to SARS-associated 62. Screaton, G., Mongkolsapaya, J., Yacoub, S. & Roberts, C. macrophages requires T cell help and is critical to trained
coronavirus after recovery. N. Engl. J. Med. 357, 1162– New insights into the immunopathology and control immunity. Cell 175, 1634–1650.e17 (2018).
1163 (2007). of dengue virus infection. Nat. Rev. Immunol. 15, 745–
46. Wu, L. P. et al. Duration of antibody responses after severe 759 (2015). Xing et al. (2020), Netea et al. (2020) and Yao et
acute respiratory syndrome. Emerg. Infect. Dis. 13, 63. Aguiar, J. A. et al. Gene expression and in situ protein al. describe the emerging concept of trained
1562–1564 (2007). profiling of candidate SARS-CoV-2 receptors in human innate immunity and suggest strategies to
47. Callow, K. A., Parry, H. F., Sergeant, M. & Tyrrell, D. A. J. The airway epithelial cells and lung tissue. Eur. Respir. J. harness this concept for developing vaccines
time course of the immune response to experimental https://doi.org/10.1183/13993003.01123-2020 (2020). against respiratory mucosal pathogens such as
coronavirus infection of man. Epidemiol. Infect. 105, 435– SARS-CoV-2.
446 (1990). 64. Mehta, P. et al. COVID-19: consider cytokine storm 86. Plotkin, S. History of vaccination. Proc. Natl Acad. Sci.
48. Chen, K. & Kolls, J. K. T cell–mediated host immune syndromes and immunosuppression. Lancet 395, USA 111, 12283–12287 (2014).
defenses in the lung. Annu. Rev. Immunol. 31, 605–633 1033–1034 (2020). 87. Almazán, F. et al. Engineering a replication-competent,
(2013). 65. Schulert, G. S. & Grom, A. A. Pathogenesis of propagation-defective middle east respiratory
49. Arunachalam, P. S. et al. T cell-inducing vaccine durably macrophage activation syndrome and potential for syndrome coronavirus as a vaccine candidate. MBio 4,
prevents mucosal SHIV infection even with lower cytokine-directed therapies. Annu. Rev. Med. 66, 145– e00650-13 (2013).
neutralizing antibody titers. Nat. Med. 26, 932–940 159 (2015). 88. Netland, J. et al. Immunization with an attenuated severe
(2020). 66. Huang, C. et al. Clinical features of patients infected with acute respiratory syndrome coronavirus deleted in E
This non-human primate study compares a vaccine 2019 novel coronavirus in Wuhan, China. Lancet 395, protein protects against lethal respiratory disease.
strategy focused on inducing neutralizing 497–506 (2020). Virology 399, 120–128 (2010).
630 | october 2020 | volume 20 www.nature.com/nri
R e v i ews
89. Hou, Y., Meulia, T., Gao, X., Saif, L. J. & Wang, Q. Deletion 108. Baden, L. R. et al. First-in-human evaluation of the safety 129. Iwata-Yoshikawa, N. et al. Effects of toll-like receptor
of both the tyrosine-based endocytosis signal and the and immunogenicity of a recombinant adenovirus stimulation on eosinophilic infiltration in lungs of
endoplasmic reticulum retrieval signal in the serotype 26 HIV-1 Env vaccine (IPCAVD 001). BALB/c mice immunized with UV-inactivated severe
cytoplasmic tail of spike protein attenuates porcine J. Infect. Dis. 207, 240–247 (2013). acute respiratory syndrome-related coronavirus
epidemic diarrhea virus in pigs. J. Virol. 93, e01758-18 109. Anywaine, Z. et al. Safety and immunogenicity of a 2- vaccine. J. Virol. 88, 8597–8614 (2014).
(2018). dose heterologous vaccination regimen with 130. Del Giudice, G., Rappuoli, R. & Didierlaurent, A. M.
90. Jimenez-Guardeño, J. M. et al. Identification of the Ad26.ZEBOV and MVA-BN-Filo Ebola vaccines: 12- Correlates of adjuvanticity: a review on adjuvants in
mechanisms causing reversion to virulence in an month data from a phase 1 randomized clinical trial licensed vaccines. Semin. Immunol. 39, 14–21 (2018).
attenuated SARS-CoV for the design of a genetically in Uganda and Tanzania. J. Infect. Dis. 220, 46–56 131. HogenEsch, H., O’Hagan, D. T. & Fox, C. B. Optimizing the
stable vaccine. PLoS Pathog. 11, e1005215 (2015). (2019). utilization of aluminum adjuvants in vaccines: you might
91. Menachery, V. D. et al. Attenuation and restoration of 110. Mercado, N. B. et al. Single-shot Ad26 vaccine protects just get what you want. NPJ Vaccines 3, 51 (2018).
severe acute respiratory syndrome coronavirus mutant against SARS-CoV-2 in rhesus macaques. Nature https://
lacking 2’-O-methyltransferase activity. J. Virol. 88, 4251– doi.org/10.1038/s41586-020-2607-z (2020). 132. Mou, H. et al. The receptor binding domain of the new
4264 (2014). Middle East respiratory syndrome coronavirus maps to a
92. Cheng, B. Y. H., Ortiz-Riaño, E., Nogales, A., 111. Ewer, K. et al. Chimpanzee adenoviral vectors as 231-residue region in the spike protein that efficiently
de la Torre, J. C. & Martínez-Sobrido, L. Development of vaccines for outbreak pathogens. Hum. Vaccin. elicits neutralizing antibodies. J. Virol. 87, 9379–9383
live-attenuated arenavirus vaccines based on codon Immunother. 13, 3020–3032 (2017). (2013).
deoptimization. J. Virol. 89, 3523–3533 (2015). 112. Folegatti, P. M. et al. Safety and immunogenicity of a 133. Guo, Y. et al. Elicitation of immunity in mice after
93. Mueller, S. et al. A codon-pair deoptimized liveattenuated candidate Middle East respiratory syndrome immunization with the S2 subunit of the severe acute
vaccine against respiratory syncytial virus is coronavirus viral-vectored vaccine: a dose-escalation, respiratory syndrome coronavirus. DNA Cell Biol. 24,
immunogenic and efficacious in non-human primates. open-label, non-randomised, uncontrolled, phase 1 510–515 (2005).
Vaccine 38, 2943–2948 (2020). trial. Lancet. Infect. Dis. 20, 816–826 (2020). 134. Zhou, Y., Jiang, S. & Du, L. Prospects for a MERS-CoV spike
94. Tao, Y. et al. Surveillance of bat coronaviruses in Kenya 113. Wilkie, M. et al. A phase I trial evaluating the safety and vaccine. Expert. Rev. Vaccines 17, 677–686 (2018).
identifies relatives of human coronaviruses NL63 and immunogenicity of a candidate tuberculosis vaccination
229E and their recombination history. J. Virol. 91, regimen, ChAdOx1 85A prime – MVA85A boost in healthy 135. Oscherwitz, J. The promise and challenge of
e01953-16 (2017). UK adults. Vaccine 38, 779–789 (2020). epitopefocused vaccines. Hum. Vaccin. Immunother. 12
95. Humphreys, I. R. & Sebastian, S. Novel viral vectors in , 2113–2116 (2016).
infectious diseases. Immunology 153, 1–9 (2018). 114. van Doremalen, N. et al. ChAdOx1 nCoV-19 vaccine 136. Du, L. et al. Recombinant receptor-binding domain of
96. Draper, S. J. & Heeney, J. L. Viruses as vaccine vectors for prevents SARS-CoV-2 pneumonia in rhesus macaques. SARS-CoV spike protein expressed in mammalian,
infectious diseases and cancer. Nat. Rev. Microbiol. 8, 62– Nature https://doi.org/10.1038/s41586-020-2608-y insect and E. coli cells elicits potent neutralizing
73 (2010). (2020). antibody and protective immunity. Virology 393, 144–
97. Cohen, J. Top U.S. scientists left out of White House 115. Folegatti, P. M. et al. Safety and immunogenicity of the 150 (2009).
selection of COVID-19 vaccine short list. Science ChAdOx1 nCoV-19 vaccine against SARS-CoV-2: a 137. Donaldson, B., Lateef, Z., Walker, G. F., Young, S. L. &
https://doi.org/10.1126/science.abd1719 (2020). preliminary report of a phase 1/2, single-blind, Ward, V. K. Virus-like particle vaccines: immunology and
98. Zhu, F.-C. et al. Safety, tolerability, and immunogenicity of a randomised controlled trial. Lancet https://doi.org/ formulation for clinical translation. Expert. Rev. Vaccines
recombinant adenovirus type-5 vectored 10.1016/S0140-6736(20)31604-4 (2020). This clinical 17, 833–849 (2018).
COVID-19 vaccine: a dose-escalation, open-label, phase I/II study evaluates a ChAdvectored COVID-19 138. Lu, X. et al. Immune responses against severe acute
non-randomised, first-in-human trial. Lancet 395, vaccine expressing the S protein, showing induction respiratory syndrome coronavirus induced by
1845–1854 (2020). of strong neutralizing antibody and overall T cell virus-like particles in mice. Immunology 122, 496–
99. Zhu, F.-C. et al. Immunogenicity and safety of a responses and representing the third published 502 (2007).
recombinant adenovirus type-5-vectored COVID-19 human COVID-19 vaccine trial in the world. This 139. Lokugamage, K. G. et al. Chimeric coronavirus-like
vaccine in healthy adults aged 18 years or older: a vaccine is the most advanced COVID-19 vaccine particles carrying severe acute respiratory syndrome
randomised, double-blind, placebo-controlled, phase candidate in terms of clinical development. coronavirus (SCoV) S protein protect mice against
2 trial. Lancet https://doi.org/10.1016/ challenge with SCoV. Vaccine 26, 797–808 (2008).
S0140-6736(20)31605-6 (2020). 116. Henao-Restrepo, A. M. et al. Efficacy and effectiveness of 140. Naskalska, A. et al. Novel coronavirus-like particles
The phase I and phase II human studies by Zhu et al. an rVSV-vectored vaccine expressing Ebola surface targeting cells lining the respiratory tract. PLoS ONE 13
evaluate an Ad5-vectored COVID-19 vaccine glycoprotein: interim results from the Guinea ring , e0203489 (2018).
expressing the S protein, representing the first vaccination cluster-randomised trial. Lancet 386, 857–866 141. Business Wire. Medicago announces positive results in
COVID-19 vaccine globally that entered clinical trials (2015). animal trials for its vaccine candidate against COVID-19.
and published results. Pre-existing vector immunity 117. Cohen, J. Merck, one of Big Pharma’s biggest players, STT https://www.sttinfo.fi/tiedote/ medicago-announces-
occurred in a significant portion of trial participants. reveals its COVID-19 vaccine and therapy plans. Science positive-results-in-animal-trialsfor-its-vaccine-candidate-
https://doi.org/10.1126/science.abd0121 (2020). against-covid-19?publisherId
100. Smaill, F. et al. A human type 5 adenovirus-based 118. Case, J. B. et al. Replication-competent vesicular stomatitis =58763726&releaseId=69881188 (2020).
tuberculosis vaccine induces robust T cell responses in virus vaccine vector protects against SARS-CoV-2- 142. Pardi, N., Hogan, M. J., Porter, F. W. & Weissman, D.
humans despite preexisting anti-adenovirus immunity. mediated pathogenesis in mice. Cell Host Microbe mRNA vaccines - a new era in vaccinology. Nat. Rev.
Sci. Transl Med. 5, 205ra134 (2013). https://doi.org/10.1016/j.chom.2020.07.018 (2020). Drug. Discov. 17, 261–279 (2018).
101. Ledgerwood, J. E. et al. A replication defective 143. Jackson, N. A. C., Kester, K. E., Casimiro, D.,
recombinant Ad5 vaccine expressing Ebola virus GP is 119. Yahalom-Ronen, Y. et al. A single dose of recombinant Gurunathan, S. & DeRosa, F. The promise of mRNA
safe and immunogenic in healthy adults. Vaccine 29, VSV-ΔG-spike vaccine provides protection against SARS- vaccines: a biotech and industrial perspective.
304–313 (2010). CoV-2 challenge. Preprint at bioRxiv https:// doi.org/ NPJ Vaccines 5, 11 (2020).
102. Gray, G. E. et al. Safety and efficacy of the HVTN 503/ 10.1101/2020.06.18.160655 (2020). 144. Lutz, J. et al. Unmodified mRNA in LNPs constitutes a
Phambili study of a clade-B-based HIV-1 vaccine in 120. Koch, T. et al. Safety and immunogenicity of a modified competitive technology for prophylactic vaccines.
South Africa: a double-blind, randomised, vaccinia virus Ankara vector vaccine candidate for NPJ Vaccines 2, 29 (2017).
placebocontrolled test-of-concept phase 2b study. Middle East respiratory syndrome: an open-label, phase 1 145. Corbett, K. S. et al. SARS-CoV-2 mRNA vaccine design
Lancet. Infect. Dis. 11, 507–515 (2011). trial. Lancet Infect. Dis. 20, 827–838 (2020). enabled by prototype pathogen preparedness. Nature
103. Xiang, Z. et al. Chimpanzee adenovirus antibodies in 121. Murdin, A. D., Barreto, L. & Plotkin, S. Inactivated https://doi.org/10.1038/s41586-020-2622-0 (2020).
humans, sub-Saharan Africa. Emerg. Infect. Dis. 12, poliovirus vaccine: past and present experience.
1596–1599 (2006). Vaccine 14, 735–746 (1996). 146. Jackson, L. A. et al. An mRNA vaccine against SARS-CoV-2 -
104. Zhu, F.-C. et al. Safety and immunogenicity of a 122. Vellozzi, C. et al. Safety of trivalent inactivated influenza preliminary report. N. Engl. J. Med. https://doi.org/
recombinant adenovirus type-5 vector-based Ebola vaccines in adults: background for pandemic influenza 10.1056/NEJMoa2022483 (2020). This clinical phase I
vaccine in healthy adults in Sierra Leone: a singlecentre, vaccine safety monitoring. Vaccine 27, 2114–2120 (2009). study evaluates an mRNA-based COVID-19 vaccine
randomised, double-blind, placebo-controlled, phase 2 expressing the S protein, showing induction of strong
trial. Lancet 389, 621–628 (2017). 123. Wood, J. M. & Robertson, J. S. From lethal virus to life- neutralizing antibody and CD4+
105. Cross, R. CanSino publishes first COVID-19 vaccine saving vaccine: developing inactivated vaccines for T cell responses in most participants and representing the
data to muted response. Chemical & Engineering pandemic influenza. Nat. Rev. Microbiol. 2, 842–847 second published human COVID-19 vaccine trial in the
News https://cen.acs.org/pharmaceuticals/vaccines/ (2004). world.
CanSino-publishes-first-COVID-19/98/i21 (2020). 124. Tahir Ul Qamar, M. et al. Epitope-based peptide vaccine 147. Mulligan, M. J. et al. Phase 1/2 study of COVID-19 RNA
106. Zhang, S. et al. Seroprevalence of neutralizing antibodies design and target site depiction against Middle East vaccine BNT162b1 in adults. Nature https:// doi.org/
to human adenoviruses type-5 and type-26 and respiratory syndrome coronavirus: an 10.1038/s41586-020-2639-4 (2020).
chimpanzee adenovirus type-68 in healthy Chinese immuneinformatics study. J. Transl Med. 17, 362 (2019). 148. Sahin, U. et al. Concurrent human antibody and TH1
adults. J. Med. Virol. 85, 1077–1084 (2013). Xiang et al. 125. Watanabe, Y., Allen, J. D., Wrapp, D., McLellan, J. S. & type T-cell responses elicited by a COVID-19 RNA
(2006) and Zhang et al. compare the prevalence of Crispin, M. Site-specific glycan analysis of the SARS- vaccine. Preprint at medRxiv https://doi. org/
pre-existing circulating neutralizing antibodies CoV-2 spike. Science 369, 330–333 (2020). 10.1101/2020.07.17.20140533 (2020).
(antivector immunity) to Ad5, Ad26 and ChAd 126. Wang, H. et al. Development of an inactivated vaccine 149. Petsch, B. et al. Protective efficacy of in vitro synthesized,
platforms in various parts of the world. The relative candidate, BBIBP-CorV, with potent protection against specific mRNA vaccines against influenza A virus
prevalence of pre-existing antivector immunity is of SARS-CoV-2. Cell 182, 713–721.e9 (2020). infection. Nat. Biotechnol. 30, 1210–1216 (2012).
importance for the choice of viral platforms. 127. Gao, Q. et al. Development of an inactivated vaccine
candidate for SARS-CoV-2. Science 369, 77–81 (2020). 150. Chahal, J. S. et al. Dendrimer-RNA nanoparticles
107. Colloca, S. et al. Vaccine vectors derived from a large generate protective immunity against lethal Ebola,
collection of simian adenoviruses induce potent cellular 128. Zeng, L. Mucosal adjuvants: opportunities and H1N1 influenza, and Toxoplasma gondii challenges
immunity across multiple species. Sci. Transl Med. 4, challenges. Hum. Vaccin. Immunother. 12, 2456– with a single dose. Proc. Natl Acad. Sci. USA 113,
115ra2 (2012). 2458 (2016). E4133–E4142 (2016).
NAture revIeWS | IMMuNOLOgy volume 20 | october 2020 | 631
R e v i ews
151. Schnee, M. et al. An mRNA vaccine encoding rabies virus cellular and humoral immune responses against SARS- 183. Wan, Y., Shang, J., Graham, R., Baric, R. S. & Li, F.
glycoprotein induces protection against lethal infection CoV-2 in mice. Immunity https://doi.org/10.1016/ Receptor recognition by the novel coronavirus from
in mice and correlates of protection in adult and j.immuni.2020.07.019 (2020). Wuhan: an analysis based on decade-long structural
newborn pigs. PLoS Negl. Trop. Dis. 10, e0004746 167. McKay, P. F. et al. Self-amplifying RNA SARS-CoV-2 lipid studies of SARS coronavirus. J. Virol. 94, e00127-20
(2016). nanoparticle vaccine candidate induces high neutralizing (2020).
152. Bahl, K. et al. Preclinical and clinical demonstration of antibody titers in mice. Nat. Commun. 11, 3523 (2020). 184. Rockx, B. et al. Comparative pathogenesis of COVID-19,
immunogenicity by mRNA vaccines against MERS, and SARS in a nonhuman primate model.
H10N8 and H7N9 influenza viruses. Mol. Ther. 25, 168. Sánchez-Ramón, S. et al. Trained immunity-based Science 368, 1012–1015 (2020).
1316–1327 (2017). vaccines: a new paradigm for the development of 185. Munster, V. J. et al. Respiratory disease in rhesus
153. Pardi, N. et al. Zika virus protection by a single lowdose broad-spectrum anti-infectious formulations. Front. macaques inoculated with SARS-CoV-2. Nature
nucleoside-modified mRNA vaccination. Nature 543, Immunol. 9, 2936 (2018). https://doi.org/10.1038/s41586-020-2324-7 (2020).
248–251 (2017). 169. Netea, M. G. et al. Defining trained immunity and its role
154. Chahal, J. S. et al. An RNA nanoparticle vaccine against in health and disease. Nat. Rev. Immunol. 20, 375–388 186. Shi, J. et al. Susceptibility of ferrets, cats, dogs, and
Zika virus elicits antibody and CD8+T cell responses in a (2020). other domesticated animals to SARS–coronavirus 2.
mouse model. Sci. Rep. 7, 252 (2017). 170. de Bree, L. C. J. et al. Non-specific effects of vaccines: Science 368, 1016–1020 (2020).
155. Alberer, M. et al. Safety and immunogenicity of a mRNA current evidence and potential implications. Semin. Together with Lakdawala and Menachery (2020), Shi
rabies vaccine in healthy adults: an open-label, non- Immunol. 39, 35–43 (2018). et al. provide information on the pros and cons of
randomised, prospective, first-in-human phase 1 clinical 171. Uthayakumar, D. et al. Non-specific effects of vaccines various animal models of COVID-19 for pathogenesis,
trial. Lancet 390, 1511–1520 (2017). illustrated through the BCG example: from immunity and vaccine studies.
156. Hobernik, D. & Bros, M. DNA vaccines—how far from observations to demonstrations. Front. Immunol. 9, 187. Zhao, X. et al. Broad and differential animal ACE2
clinical use? Int. J. Mol. Sci. 19, 3605 (2018). 2869 (2018). receptor usage by SARS-CoV-2. J. Virol. https://
157. Smith, T. R. F. et al. Immunogenicity of a DNA vaccine 172. Kaufmann, E. et al. BCG educates hematopoietic stem doi.org/10.1128/JVI.00940-20 (2020).
candidate for COVID-19. Nat. Commun. 11, 2601 (2020). cells to generate protective innate immunity against 188. Bao, L. et al. The pathogenicity of SARS-CoV-2 in
tuberculosis. Cell 172, 176–190.e19 (2018). hACE2 transgenic mice. Nature 583, 830–833
158. Yu, J. et al. DNA vaccine protection against SARS- 173. Cirovic, B. et al. BCG vaccination in humans elicits (2020).
CoV-2 in rhesus macaques. Science https:// doi.org/ trained immunity via the hematopoietic progenitor
10.1126/science.abc6284 (2020). compartment. Cell Host Microbe https://doi.org/ Acknowledgements
159. Lichty, B. D., Breitbach, C. J., Stojdl, D. F. & Bell, J. C. Going 10.1016/j.chom.2020.05.014 (2020). The work was supported by the Canadian Institutes of Health
viral with cancer immunotherapy. Nat. Rev. Cancer 14, 174. Arts, R. J. W. et al. BCG vaccination protects against Research (CIHR) COVID-19 Rapid Research Program, the CIHR
559–567 (2014). experimental viral infection in humans through the Foundation Program, the National Sanitarium Association of
160. Mohn, K. G.-I., Smith, I., Sjursen, H. & Cox, R. J. Immune induction of cytokines associated with trained Canada Innovative Research Program, the Natural Sciences
responses after live attenuated influenza vaccination. immunity. Cell Host Microbe 23, 89–100.e5 (2018). and Engineering Research Council of Canada, the Canadian
Hum. Vaccin. Immunother. 14, 571–578 (2018). 175. Verrall, A. J. et al. Early clearance of mycobacterium Foundation for Innovation, Ontario Government, and
tuberculosis is associated with increased innate McMaster University.
161. Low, N. et al. A randomized, controlled trial of an immune responses. J. Infect. Dis. 221, 1342–1350
aerosolized vaccine against measles. N. Engl. J. Med. (2019).
Author contributions
372, 1519–1529 (2015). 176. Moorlag, S. J. C. F. M., Arts, R. J. W., van Crevel, R. &
The authors contributed equally to all aspects of the article.
162. Satti, I. et al. Safety and immunogenicity of a candidate Netea, M. G. Non-specific effects of BCG vaccine on
tuberculosis vaccine MVA85A delivered by aerosol in viral infections. Clin. Microbiol. Infect. 25, 1473–1478
Competing interests
BCG-vaccinated healthy adults: a phase 1, double-blind, (2019).
The authors declare no competing interests.
randomised controlled trial. Lancet Infect. Dis. 14, 939– 177. Covián, C., Retamal-Díaz, A., Bueno, S. M., Kalergis, A.
946 (2014). Mohn et al. (2018), Low et al. (2015) and M. & Could, B. C. G. Vaccination induce protective
Peer review information
Satti et al. provide three successful examples of trained immunity for SARS-CoV-2? Front. Immunol. 11,
Nature Reviews Immunology thanks P. Klenerman and the
implementing respiratory mucosal delivery of virus- 970 (2020).
other, anonymous, reviewer(s) for their contribution to the
based vaccines to humans, each against a different 178. O’Neill, L. A. J. & Netea, M. G. BCG-induced trained
peer review of this work.
type of respiratory mucosal pathogen. immunity: can it offer protection against COVID-19?
Nat. Rev. Immunol. 20, 335–337 (2020). This is an
163. Burton, D. R. & Walker, L. M. Rational vaccine design in overview of the current global effort in clinically Publisher’s note
the time of COVID-19. Cell Host Microbe 27, 695–698 testing the potential non-specific protective effect Springer Nature remains neutral with regard to jurisdictional
(2020). of BCG, a human TB vaccine, on controlling claims in published maps and institutional affiliations.
164. World Economic Forum. 3 challenges in creating a COVID-19 infection and severity, based on the
coronavirus vaccine – and how they are being concept of trained innate immunity.
overcome. World Economic Forum https://www. 179. Ordovas-Montanes, J., Beyaz, S., Rakoff-Nahoum, S. & RelateD lINks
weforum.org/agenda/2020/05/coronavirus-covid-19- Shalek, A. K. Distribution and storage of Australian New Zealand Clinical Trials Registry (ANZCTR):
vaccine-industry/ (2020). inflammatory memory in barrier tissues. Nat. Rev. http://www.anzctr.org.au/
This commentary identifies the three biggest Immunol. 20, 308–320 (2020). Chinese Clinical Trial Registry (ChiCTR): http://www.chictr.
hurdles to COVID-19 vaccine development and 180. Cardani, A., Boulton, A., Kim, T. S. & Braciale, T. J. org.cn/index.aspx
vaccination implementation as developing and Alveolar macrophages prevent lethal influenza ClinicalTrials.gov: https://clinicaltrials.gov/ eU Clinical
selecting the safest and most effective vaccine, pneumonia by inhibiting infection of type-1 alveolar Trials Register (eudraCT): https://www.
acquiring large-scale manufacturing capacities and epithelial cells. PLoS Pathog. 13, e1006140 (2017). clinicaltrialsregister.eu/
ensuring transparent and fair vaccine distribution. 181. Guillon, A. et al. Pneumonia recovery reprograms the isRCTN registry: https://www.isrctn.com/
165. Bollyky, T. J., Gostin, L. O. & Hamburg, M. A. The alveolar macrophage pool. JCI Insight 5, e133042 Pan African Clinical Trials Registry (PACTR): https://pactr.
equitable distribution of COVID-19 therapeutics and (2020). samrc.ac.za/
vaccines. JAMA 323, 2462 (2020). 182. Lakdawala, S. S. & Menachery, V. D. The search for a
166. Laczkó, D. et al. A single immunization with COVID-19 animal model. Science 368, 942–943 (2020).
nucleoside-modified mRNA vaccines elicits strong © Springer Nature Limited 2020
632 | october 2020 | volume 20 www.nature.com/nri
Anda mungkin juga menyukai
- Mikrobiologi Perubatan I: Patogen dan Mikrobiologi ManusiaDari EverandMikrobiologi Perubatan I: Patogen dan Mikrobiologi ManusiaPenilaian: 2.5 dari 5 bintang2.5/5 (2)
- KELOMPOK XX - Karya Ilmiah Efek Vaksin Bagi Civitas UkwmsDokumen10 halamanKELOMPOK XX - Karya Ilmiah Efek Vaksin Bagi Civitas UkwmsTeresa ThamyBelum ada peringkat
- Bahan Vaksin Covid-19Dokumen28 halamanBahan Vaksin Covid-19NovaWulandariPalufiBelum ada peringkat
- Power Point Vaksin CovidDokumen60 halamanPower Point Vaksin CovidLUSY KRITLINABelum ada peringkat
- Vaksin Covid Ed1-1Dokumen9 halamanVaksin Covid Ed1-1ferry gunawanBelum ada peringkat
- Vaksin Covid - Tinjauan Kepustakaan - DR Dominicus HusadaDokumen15 halamanVaksin Covid - Tinjauan Kepustakaan - DR Dominicus HusadaSahad BayuBelum ada peringkat
- Bab Ii CJRDokumen5 halamanBab Ii CJRahyana rehaniBelum ada peringkat
- Metopen RismaayufitriaDokumen9 halamanMetopen RismaayufitriaAnnisa LuthfiaBelum ada peringkat
- REFERAT Vaksin Covid-19 IKM-IKK HALISA RAHMASARI 11120192137Dokumen28 halamanREFERAT Vaksin Covid-19 IKM-IKK HALISA RAHMASARI 11120192137gufranBelum ada peringkat
- Point 4Dokumen10 halamanPoint 4Luthfi PrayogiBelum ada peringkat
- Jurnal Mekanisme VaksinDokumen13 halamanJurnal Mekanisme VaksinReza FahriBelum ada peringkat
- Bab 1Dokumen7 halamanBab 1Jordan HutabaratBelum ada peringkat
- Nova Aulia Putri A - 22 - XI MIPA 3 - Makalah Efektivitas Vaksinasi Covid-19Dokumen9 halamanNova Aulia Putri A - 22 - XI MIPA 3 - Makalah Efektivitas Vaksinasi Covid-19SALSABELA ALMIRABelum ada peringkat
- Tugas Self Learning - Analisis Isu InstansiDokumen5 halamanTugas Self Learning - Analisis Isu InstansiputzaiputriBelum ada peringkat
- LKS PLHDokumen14 halamanLKS PLHEriel EmerioBelum ada peringkat
- 142-Article Text-911-1-10-20221202Dokumen8 halaman142-Article Text-911-1-10-20221202SyairoziBelum ada peringkat
- BAB AkhirDokumen1 halamanBAB Akhiranandaazaliaputri11Belum ada peringkat
- LEMBAR KERJA SISWA Virus Corona OK 2Dokumen18 halamanLEMBAR KERJA SISWA Virus Corona OK 2NIABelum ada peringkat
- 177-Article Review-1292-1-10-20220209Dokumen6 halaman177-Article Review-1292-1-10-20220209Alung GantengBelum ada peringkat
- BEC - Cindi Kartika Dan Rahma Sari Natasya - S1 Farmasi - Vaksin Terhadap Kesehatan - Rahma NatasyaDokumen7 halamanBEC - Cindi Kartika Dan Rahma Sari Natasya - S1 Farmasi - Vaksin Terhadap Kesehatan - Rahma NatasyaHilda FauziahBelum ada peringkat
- Tugas Kelompok Ekopolgob - Press Release KemenluDokumen11 halamanTugas Kelompok Ekopolgob - Press Release Kemenlunabila annisa putriBelum ada peringkat
- Agus Salim - Revisi Analisis Jurnal - LKMMD 3Dokumen8 halamanAgus Salim - Revisi Analisis Jurnal - LKMMD 3Agus SalimBelum ada peringkat
- Tugas Biologi Covid-19. Muhamad Deny Firmansyah XI MIPADokumen10 halamanTugas Biologi Covid-19. Muhamad Deny Firmansyah XI MIPADeny GameBelum ada peringkat
- Tugas IndividuDokumen8 halamanTugas IndividuMusdaliva Tri Riskiani AlminBelum ada peringkat
- Laporan KBM Di Rumah Sman 5 CirebonDokumen21 halamanLaporan KBM Di Rumah Sman 5 CirebonindrayusufgeoBelum ada peringkat
- 684 1147 1 SMDokumen20 halaman684 1147 1 SMNada LathifahBelum ada peringkat
- Tinjauan PustakaDokumen15 halamanTinjauan PustakaJoy FeriantoBelum ada peringkat
- Alfira X Mipa 2 Lembar Kerja SiswaDokumen19 halamanAlfira X Mipa 2 Lembar Kerja Siswasalwa huzaifahBelum ada peringkat
- Makalah Biologi - Mega Rohmah D.Dokumen9 halamanMakalah Biologi - Mega Rohmah D.SALSABELA ALMIRABelum ada peringkat
- TGSDokumen15 halamanTGSdinda malaBelum ada peringkat
- Lukman Wahid (Kls A)Dokumen10 halamanLukman Wahid (Kls A)Lukman WahidBelum ada peringkat
- 1648 6082 2 PBDokumen25 halaman1648 6082 2 PBAryo PBelum ada peringkat
- Vaksin CovidDokumen11 halamanVaksin CovidRadhwa FauztinaBelum ada peringkat
- Proposal Penelitian1 - DM - RR - Revisi 4Dokumen27 halamanProposal Penelitian1 - DM - RR - Revisi 4Dhea HuseinBelum ada peringkat
- Lembar Kerja Siswa Covid-19Dokumen13 halamanLembar Kerja Siswa Covid-19arina putriBelum ada peringkat
- Bahasa IndonesiaDokumen14 halamanBahasa IndonesiaVENI VITRIANIBelum ada peringkat
- Bab Ii BioteknologiDokumen4 halamanBab Ii Bioteknologiarimbi fairuzBelum ada peringkat
- VaksinasiDokumen60 halamanVaksinasiHardianto Eko Jabaka NaghBelum ada peringkat
- KTI - Ike FixDokumen14 halamanKTI - Ike Fixmaselayona418Belum ada peringkat
- FARMAKOTERAPI IKA NURFAHMI-5aDokumen12 halamanFARMAKOTERAPI IKA NURFAHMI-5aIka NurFahmiiBelum ada peringkat
- Materi PBLDokumen10 halamanMateri PBLAde CahyatiBelum ada peringkat
- NaskahDokumen12 halamanNaskahYudha FerriansyahBelum ada peringkat
- MiniproDokumen34 halamanMiniproalvinBelum ada peringkat
- Willingness To Pay For A COVID 19 Vaccine and Its Associated Determinants in Indonesia - En.idDokumen8 halamanWillingness To Pay For A COVID 19 Vaccine and Its Associated Determinants in Indonesia - En.idgifa maulinasariBelum ada peringkat
- Jurnal Skripsi NurDokumen16 halamanJurnal Skripsi NurnanaBelum ada peringkat
- Minipro NadiaDokumen45 halamanMinipro NadiaalvinBelum ada peringkat
- 156-Article Text-309-1-10-20211016Dokumen5 halaman156-Article Text-309-1-10-20211016St MarwahBelum ada peringkat
- Kelompok 2 Proposal PenelitianDokumen15 halamanKelompok 2 Proposal Penelitianika dilapangaBelum ada peringkat
- Proposal Penelitian Kel. 7 - Nabila Annisa Putri (6211191007, Kls A)Dokumen15 halamanProposal Penelitian Kel. 7 - Nabila Annisa Putri (6211191007, Kls A)nabila annisa putriBelum ada peringkat
- Panduan Untuk Vaksin Dan ObatDokumen11 halamanPanduan Untuk Vaksin Dan ObatMon RoeBelum ada peringkat
- It VaksinDokumen4 halamanIt VaksinMuhamad noval HabibiBelum ada peringkat
- Apakah Vaksin COVIDDokumen5 halamanApakah Vaksin COVIDPuskesmas Perawatan MenawiBelum ada peringkat
- Analisis Faktor Health Belief Model Pada Penerimaan Vaksinasi Covid-19Dokumen5 halamanAnalisis Faktor Health Belief Model Pada Penerimaan Vaksinasi Covid-19Beta RaeBelum ada peringkat
- Vaccines-09-00941 en IdDokumen16 halamanVaccines-09-00941 en IdWinatta SariiBelum ada peringkat
- Artikel 1Dokumen11 halamanArtikel 1Widiyatul FitrianiBelum ada peringkat
- Soal Ujian Akhir Semester EpidemiologiDokumen10 halamanSoal Ujian Akhir Semester EpidemiologizachryekelBelum ada peringkat
- Kuliah Pertemuan 2. COVID-19 (Sekolah Tinggi Farmasi Indonesia) 2021Dokumen68 halamanKuliah Pertemuan 2. COVID-19 (Sekolah Tinggi Farmasi Indonesia) 2021Muhammad nandiBelum ada peringkat
- Jurnal Sistem Imun (Riska)Dokumen12 halamanJurnal Sistem Imun (Riska)Riska Novia RachmanBelum ada peringkat
- D4 PBL 20 Sken 10Dokumen20 halamanD4 PBL 20 Sken 10Togu JastinBelum ada peringkat
- 176-Article Review-984-1-10-20210719Dokumen4 halaman176-Article Review-984-1-10-20210719astri yuliyaBelum ada peringkat
- 741 1829 1 PBDokumen8 halaman741 1829 1 PBDeys AmirBelum ada peringkat
- New Kemasan AmpulDokumen2 halamanNew Kemasan AmpulDeys AmirBelum ada peringkat
- 1211 4740 1 PBDokumen6 halaman1211 4740 1 PBDeys AmirBelum ada peringkat
- 190 430 1 SMDokumen5 halaman190 430 1 SMDeys AmirBelum ada peringkat
- New Kemasan AmpulDokumen2 halamanNew Kemasan AmpulDeys Amir100% (1)
- 7 Asmiati NewDokumen6 halaman7 Asmiati NewDeys AmirBelum ada peringkat
- New Kemasan Ampul Terbaru Skali-1Dokumen2 halamanNew Kemasan Ampul Terbaru Skali-1Deys AmirBelum ada peringkat
- New Kemasan Ampul Terbaru SkaliDokumen2 halamanNew Kemasan Ampul Terbaru SkaliDeys AmirBelum ada peringkat
- Daftar PustakaDokumen1 halamanDaftar PustakaDeys AmirBelum ada peringkat
- Cover BioselDokumen1 halamanCover BioselDeys AmirBelum ada peringkat
- Kata PengantarDokumen3 halamanKata PengantarDeys AmirBelum ada peringkat
- Kata PengantarDokumen3 halamanKata PengantarDeys AmirBelum ada peringkat
- Daftar PustakaDokumen1 halamanDaftar PustakaDeys AmirBelum ada peringkat
- Mual Muntah Kel. 7Dokumen27 halamanMual Muntah Kel. 7Deys AmirBelum ada peringkat
- Alkes Kel 20Dokumen3 halamanAlkes Kel 20Deys AmirBelum ada peringkat
- Titrasi Asam BasaDokumen16 halamanTitrasi Asam BasaDeys AmirBelum ada peringkat